ON CALL NEURO

ON CALL NEURO aims to provide residents with a quick “guide” to handling neurological cases and consults while on service or on call.This guide is not a replacement for understanding concepts in neurology in depth. However, it does provide a quick summary of pertinent clinical information and a reference for management algorithms and treatment options.This website's intended audience is for medical providers for educational purposes only. It is not meant to be used as medical advice for the general public. Please see the disclaimer for further information.If you have any feedback for the website, please fill out the survey here.
Approach to...
COMING SOON
Approach to... is a new section that will provide approaches to various undifferentiated cases (e.g. weakness, dizziness, and diplopia) Check back soon for when this section launches.
Headache
Important to rule out secondary headache causes from primary headache disorders using SNOOP4
| Clinical Features | Differential Diagnosis | |
|---|---|---|
| S | Systemic symptoms (e.g. weight loss, fevers) | Malignancy, infections, GCA |
| N | Neurological symptoms (e.g. focal neurological symptoms, confusion vision loss) | Structural lesions, strokes, encephalitis |
| O | Older age (Over 50) | Mass lesions, GCA |
| O | Onset ("Thunderclap" like, maximal intensity in less than a minute) | Vascular causes (e.g. SAH, RCVS, hemorrhagic stroke) |
| P | Papilledema | Raised ICP (IIH) |
| P | Pregnancy | Pre-eclampsia, CVST, RCVS |
| P | Positional (e.g. worse with Valsalva or worse from supine to sitting) | SIH, CVST, mass lesions |
| P | Pattern change (change in headache pattern or quality) | Assess other secondary causes |
Migraines & Tension Headaches
By Dr. Andrea Kuczynski and Dr. Caz Zhu
Reviewed by Dr. Will Kingston
Migraines
Pathophysiology and Epidemiology
Activation of trigeminal vascular system and cortical spreading depression
Affects people in their peak productive years. Second most disabling condition, second only to low back pain
More common in females, strong family history present
Clinical Features
5 or more attacks
Lasting 4hrs to 3 days
With 2 of the following: unilateral, pulsating/throbbing quality, moderate to severe intensity, worse with activity
With 1 of: photo/phonophobia or nausea/vomiting
Aura lasting 5 to 60min before headache onset, accompanied or followed by headache within 60min. Symptoms of aura are fully reversible and can present as sensory (e.g. numbness/parasthesias), visual, speech and/or language, motor, or brainstem (rare) features
⊙ CLINICAL PEARL
Three best clinical clues to diagnosis migraines: PIN the diagnosis - Photophobia, impairing, and nausea
Investigations
Neuroimaging is needed if red flags are present
Unusual, prolonged, or persistent aura
Increasing frequency, severity, or change in migraine clinical features unless change in pattern (i.e. medication overuse headache)
First or worst migraine
Migraine with brainstem aura
Confusional migraine
Hemiplegic migraine
Late-life migrainous accompaniments - acephalgic migraine
Migraine aura without headache
Side-locked migraine
Post-traumatic migraine
Treatment
Abortive therapy: NSAIDs (e.g. Ibuprofen, Naproxen 250-500mg p.o. with PPI, Cambia 1 sachet p.o.), Tylenol, triptans, Mg can be taken with aura to try and reduce its duration and severity, Ubrogepant (CGRP antagonist) - 50-100 mg daily is a new approved medication for an abortive agent (side effects: nausea, drowsiness)
Acute therapy in the ED: normal saline 2-3L IV bolus (ensure no CHF), metoclopramide 10mg IV (check QTc interval), Mg 1g IV, Ketorolac 15-30mg IV, DHE 0.5mg IV with metoclopramide and if tolerated can receive 1mg as next dose (contraindicated if triptan use within 24 hours; check QTc interval)
Preventative therapy: started when >4 headache days/month and/or no response to acute therapy, and the choice depends on comorbidities and symptoms
CGRP antagonists can be considered in outpatient follow-up as a preventative therapy
Lidocaine nerve block (+/- methylprednisone) acts as both acute and preventative therapies
Nutraceuticals: Mg 300-600mg qhs, vitamin D 1000-2000IU, riboflavin 400mg, coenzyme Q10 300mg daily
Non-pharmacological therapy: reduce lifestyle triggers, relaxation/meditation, massage, exercise, reduce caffeine intake, increase hydration, protein-rich diet (especially breakfast), Cephaly device, mindfulness
Medication overuse headache (>15 days/month of NSAID/Tylenol use and/or >10 days/month of triptan use) therapy: discontinue NSAIDs/Tylenol, attempt to break the headache cycle with a longer acting NSAID (e.g. Anaprox 550mg BID or Naproxen 250-500mg BID) x1-2 weeks
Note: Lidocaine nerve block (+/- methylprednisone) and Botox injections act as both acute and preventative therapies
TRIPTANS
| Triptan | Medication Dose | Uses | Side-effects |
|---|---|---|---|
| Almotriptan | 12.5mg p.o | Good for patients with significant side effects from previous triptans | Lowest side-effect profile; Mild stiffness |
| Sumatriptan | 25-50mg p.o, 5-10mg intra-nasal, 4-6mg SC | Nasal options are best for patients with rapid onset/wake-up headaches; Only triptan with an injectable option | Bad taste, burning sensation (intra-nasal and SC), tingling, injection site reaction, nausea/vomiting |
| Rizatriptan | 5-10mg p.o./MLT | MLT option is useful for patients with strong components of nausea | Lowest risk of medication overuse headaches;; Dizziness, somnolence, dry mouth, asthenia |
| Zolmitriptan | 2.5-10mg p.o./MLT, 5mg intra-nasal | MLT option is useful for patients with strong components of nausea; Nasal options are best for patients with rapid onset/wake-up headaches | Nausea/vomiting, paraesthesias, somnolence, nasal discomfort |
| Frovatriptan | 2.5mg p.o. | Menstrually-related migraine (used on day -2 or -3 of menses) | GI upset, nausea/vomiting |
| Naratriptan | 2.5mg p.o. | Menstrually-related migraine (used on day -2 or -3 of menses) | GI upset, nausea/vomiting |
| Eletriptan | 40mg p.o. | - | Lowest risk of Medication overuse headaches; Dizziness, somnolence, dry mouth, asthenia |
Contraindications of triptans:
MAO inhibitor within 2 weeks
CAD, vasculopathy, PVD
Cardiac arrhythmia
Recent stroke
Uncontrolled HTN
Renal disease
Anaphylaxis to triptans previously
Hemiplegic migraine
Migraine with brainstem aura
Intake of ergots or triptans within 24 hours
PREVENTIVE MEDICATIONS FOR MIGRAINES
| Medication | Dose | Considerations | Side-effects |
|---|---|---|---|
| Candesartan | 2mg p.o. daily with up-titration by 2mg weekly (maximum 16mg/day) | Comorbid HTN; Contraindicated in pregnancy | Hypotension, dizziness |
| Propranolol | 40-80mg p.o daily and uptitrate up to 240mg/day | Avoid in patients with asthma or heart block; Comorbid anxiety | Hypotension, dizziness |
| Gabapentin | 300mg p.o. daily/TID with up-titration by 300mg weekly targeting 1200-1500mg/day divided TID (max 1800mg/day) | Avoid in renal failure; Sleep disturbances, mood, neuropathy | Drowsiness, dizziness |
| Topiramate | 15-25mg p.o. daily with up-titration by 15-25mg q1-2weeks targeting 100mg qhs or 50mg BID (max 200mg/day) | Comorbid mood disturbances; Contraindicated in pregnancy | Nephrolithiasis, acute closure glaucoma, dizziness, tremor, cognitive slowing, weight loss |
| Nortriptyline | 10mg p.o. Qhs with up-titration of 10mg q1-2weeks targeting 20-40mg daily (maximum 150 mg/day) | Sleep disturbances, mood | Weight gain, drowsiness, increased seizure threshold |
| Amitriptyline | 10mg p.o. Qhs with up-titration of 10mg q1-2weeks targeting 20-40mg daily (maximum 150 mg/day) | Comorbid anxiety/depression | Weight gain, drowsiness, increased seizure threshold |
| Atojepant | 5mg/kg p.o. daily | - | Constipation, nausea |
CGRP antagonists (erenumab, fremanezumab, galcanezumab) are options for treating migraines as well - although currently, indicated for patients who have headaches ≥ 8 headache days/months and have failed or are intolerant to ≥ 2 preventative agents. Side effects of CGRP antagonists include constipation, injection site reaction, and hypertension (erenumab).
Patient Education
Encourage patients to keep track of the frequency and intensity of their migraines (Migraine Tracker app)
Patients should be taking abortive therapies EARLY (as soon as they feel like they are getting their migraine) to prevent central sensitization
If their migraines continue to persist - they can take another NSAID or triptan in another 2 hours
Not all triptans are effective for everyone; just because one triptan is not effective does not mean another will not be for the patient
If a patient still experiences high intensity of migraine after taking a triptan, a second dose can be taken 2 hours after the first dose (maximum 2 doses in 24 hours)
Preventative therapy can take 2-3 months to see benefits and often can be up-titrated as tolerated
Treatment of comorbid conditions (e.g. depression) is important
Tension Type Headaches
Important to note that many people diagnosed with tension type headaches are mis-diagnosed migraines
Clinical Features
Can last hours to days
With 2 of the following: bilateral, pressing/tightening (non-pulsatile), mild or moderate intensity, not worse with activity
No more than 1 of photophobia, phonophobia, or mild nausea
Considered a chronic tension type headache if it occurs < 15 days a month or > 3 months
If a patient presents to the physician/hospital with TTH, re-think the diagnosis
Investigations & Treatment
See above section for migraines
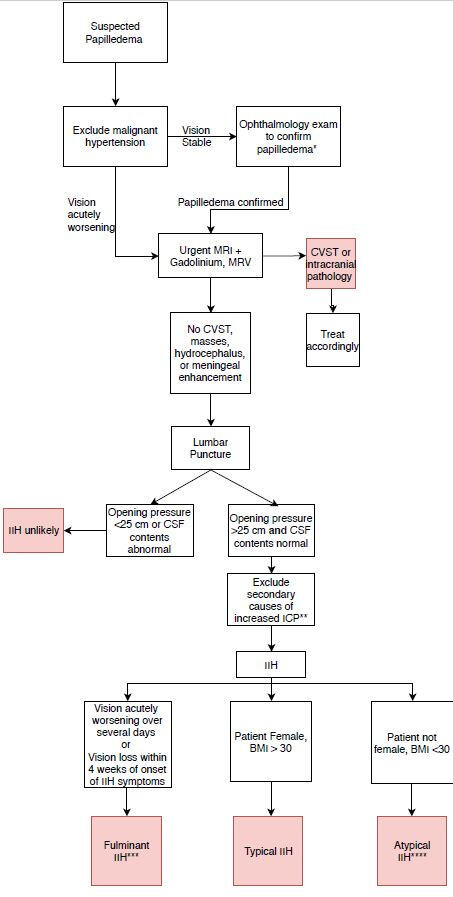
Idiopathic intracranial hypertension
By Dr. Kia Gilani
Reviewed by Dr. Jonathan Micieli and Dr. Will Kingston
Pathophysiology and Epidemiology
Raised ICP without the presence of a space-occupying lesion
Thought to be related to reduced CSF absorption
More common in females of child-bearing age
Clinical Features
Headache
Transient visual obscurations - unilateral or bilateral greying of vision or dark spots that are worse when bending over or Valsalva
Blurry vision
Horizontal diplopia - CN6 palsy
Reduced visual acuity in some (less common)
Pulsatile tinnitus
Back and/or neck pain
Radicular pain
Cognitive disturbance
ICHD criteria for Headache attributed to IIH
New headache or significant worsening of pre-existing headache
Both of: IIH diagnosis, and CSF opening pressure >25 cmH2O
Either of: headache developed or significantly worsened in relation to IIH or led to its diagnosis; headache accompanied by either or both of pulsatile tinnitus, papilledema
Not better accounted for by other ICHD-3 criteria
Click image to enlarge
Must rule out secondary causes of increased ICP
CVST
Medications: antibiotics (tetracyclines, fluoroquinolones), vitamin A derivatives, lithium, thyroxine in children, corticosteroids
SVC obstruction (very rare)
Associations with IIH:
Endocrine: PCOS, Cushing’s, Addison’s, hypoparathyroidism, hypothyroidism
Polycythemia, anemia
Uremia and/or renal failure
OSA
SLE
Down’s syndrome, Turner’s syndrome
Investigations
CBC
MRI/MRV brain or acutely CT/CTV brain if MRI unavailable
Consult/refer to Ophthalmology
Lumbar puncture with opening pressure in supine position
Blood pressure
Common neuroimaging findings in IIH
Optic nerve tortuosity
Enlarged optic nerve sheath
Flattened posterior globe
Intraocular protrusion of optic nerve head
Empty sella
Bilateral transverse sinus stenosis
Slit-like ventricles
Acquired tonsillar ectopia
Treatment
Weight loss; consider referral to bariatric clinic
Low sodium diet
Acetazolamide 500mg p.o. BID (up to 4000mg/day) - titrated by Ophthalmology based on degree of papilledema and visual function
Topiramate
Discontinue offending agent if present; treat underlying cause if present
Management of comorbidities (i.e. OSA)
Surgery in fulminant cases: VP shunting, optic nerve sheath fenestration, sinus stenting
Patient Education
Treatment is aimed at visual sparing and persistence of headache should not be considered treatment failure
Patients should be counseled on the importance of weight loss, as it is the most common risk factor and the only disease modifying treatment available
The importance of adequate follow up should be emphasized, as untreated IIH can cause permanent vision loss
Up to 40% of patients may have recurrence
Spontaneous Intracranial Hypotension
By Dr. Caz Zhu
Reviewed by Dr. Will Kingston
Pathophysiology and Epidemiology
Caused by CSF leakage, diagnosis requires presence of low CSF pressure and/or evidence of CSF leak on imaging
Female predominance (2:1) and in patients in their 30-50's
Clinical Features
Orthostatic headaches (develops when upright and improves with lying supine) - orthostatic features may disappear if SIH has been longstanding
Other symptoms include: nausea/vomiting, hypoacusis, neck stiffness/pain, tinnitus, other neurological symptoms if due to downward displacement of the brain (e.g. diplopia, gait changes)
Can also be seen in unexplained coma
ICHD criteria for Headache attributed to SIH
Headache fulfilling criteria for 7.2 Headache attributed to low cerebrospinal fluid (CSF) pressure (see below)
Absence of a procedure or trauma known to be able to cause CSF leakage (Cannot be diagnosed within 30 days of a spinal tap)
Headache has developed in temporal relation to occurrence of low CSF pressure or CSF leakage, or has led to its discovery
Not better accounted for by another ICHD-3 diagnosis
Headache attributed to low CSF pressure
Either or both of the following:
Low CSF pressure (<60 mm CSF)
Evidence of CSF leakage on imaging
Investigations
MRI/MRV brain and spine
Consider CT Myelogram or Digital Subtraction Myelography - helpful to localize CSF leak
Lumbar puncture with opening pressure in supine position (may not be necessary if enough clinical suspicion)
Common neuroimaging findings in SIH
Subdural collections
Enhancement of pachymeninges
Engorgement of venous structure
Pituitary enlargement
Sagging of brain (can ask radiology to look specifically for mammilopontine distance)
Subdural collection and hematomas
Treatment
Conservative: Bed rest, hydration, NSAIDs, caffeine
Epidural blood patch or fibrin glue patch (intrathecal infusion of 20 - 130 cc of blood) - will need to consult anesthesiology - however only 1/3 patients respond to first patch
Surgical referral if three failed blood patches
Trigeminal autonomic cephalalgias
By Dr. Caz Zhu
Reviewed by Dr. Will Kingston
Pathophysiology and Epidemiology
Male to female predominance (3:1) only in cluster headaches
Unclear pathophysiology - thought to be related to trigeminal autonomic reflex (trigeminovascular system, occipital nerves, thalamus and hypothalamus)
Most causes are primary but important to rule out secondary causes of cluster headaches including vascular & masses (carotid artery dissections, cavernous meningioma, pituitary adenomas)
More pituitary lesions seen in people with cluster headaches
Clinical Features
Often side-locked headaches with unilateral autonomic symptoms (lacrimation, red eye, ptosis/eye edema, nasal congestion, sweating/flushing)
Associated with restlessness/agitation (banging head on wall, rocking), not able to sit still during an attack
Four common TACS:
| TACS | Cluster Headaches | Short-lasting Unilateral Neuralgiform headache attacks with Conjunctival injection and Tearing (SUNCT) |
|---|---|---|
| Clinical characteristics | Unilateral side-locked headaches, “suicide headaches”, often “wake-up” headaches and occur seasonally | Prominent autonomic symptoms, +++ frequent and short-lived |
| ICHD-3 | At least 5 attacks that are severe, unilateral orbital/supraorbital, temporal pain lasting 15-180 minutes; unilateral autonomic symptoms and/or restless or agitation; occurring every other day - 8 attacks/day | At least 20 attacks that are moderate - severe pain in orbital, supraorbital, temporal, trigeminal distribution lasting 1 - 600 seconds as stabbing/saw-tooth pattern; unilateral autonomic symptoms; occurring once a day up to half the time |
| TACS | Paroxysmal Hemicrania | Hemicrania Continua |
|---|---|---|
| Clinical characteristics | Similar to cluster headaches but shorter and less restlessness. Responds to indomethacin | Constant, side locked headache, occasional migrainous features due to constant nature. Responds to indomethacin |
| ICHD-3 | At least 20 attacks that are severe, unilateral, orbital, supraorbital, temporal pain lasting 2 - 30 minutes; unilateral autonomic symptoms; occurring 5 attacks/day or more than half the time; attacks prevented by indomethacin | Unilateral headache that is present for more than 3 months with exacerbations of moderate/great intensity, can be remitting (pain remission for 1 day) or unremitting (no pain remission for 1 day for at least 1 year), attacks prevented by indomethacin |
Investigations
MRI brain with sella views +/- vascular imaging (MRA)
Hormonal testing - testosterone
Sleep study
Treatment
Cluster Headache treatment classified as abortive, transitional, and preventative treatment
| Abortive Therapy | Transitional Therapy | Preventative Therapy |
|---|---|---|
| High flow oxygen (12-15 L/NRB), Intranasal Zolmitriptan 5-10 mg, Intranasal Sumatriptan 20 mg, Intranasal lidocaine | Suboccipital steroid injection, Corticosteroids (prednisone/dexamethasone), Naratriptan, possibly IV corticosteroids for refractory cases | Galcazemuab, Level C evidence but verapamil, lithium, warfarin, melatonin, and gabapentin (high dose, non-invasive vagal nerve stimulation |
Paroxysmal Hemicrania and Hemicrania Continua: Indomethacin (up to 75 mg TID) and/or Melatonin
Indomethacin trial: Start with 25 mg TID for 1 week, then increase by 25 mg TID per week until final dose of 75 mg TID. If headaches are eliminated, then slowly remove one tablet per week until you reach the lowest effective dose for headache improvement. PPI is also recommended.
SUNCT: Lamotrigine is 1st line, then topiramate, gabapentin/pregabalin, verapamil, methylprednisolone
Secondary causes of cluster headaches: Medical or surgical treatment of lesion can improve headaches
Trigeminal Neuralgia
By Dr. Andrea Kuczynski
Reviewed by Dr. Will Kingston
Pathophysiology and Epidemiology
Must rule out post-herpetic neuralgia
Usually middle age, females affected more
May be secondary to MS lesions (especially if bilteral)
Clinical Features
Greater than or equal to 3 attacks
Recurrent sudden onset paroxysmal attacks lasting <2min that are severe, described as electrical shocks, shooting, sharp pain
Affecting the greater than or equal to 1 trigeminal nerve distribution unilaterally (V2 and V3 are more common than V1)
Pain with innocuous stimuli (eating, brushing teeth, shaving, wind blowing on face)
Refractory period: period of time where repetitive innocuous stimuli do not aggravate the attack; not a feature in TACs
Investigations
Can consider MRI brain with trigeminal nerve protocol to visualize is there is any vascular compression of the nerve
Treatment
Acute treatment in the ED: Phenytoin 15 mg/kg IV over 30 minutes or Lacosamide 100 mg IV
Carbamazepine 200-1200 mg/day
Gabapentin or Pregabalin
Gamma knife radiosurgery (if refractory to medical treatment)
Surgical decompression of nerve if evident pathology
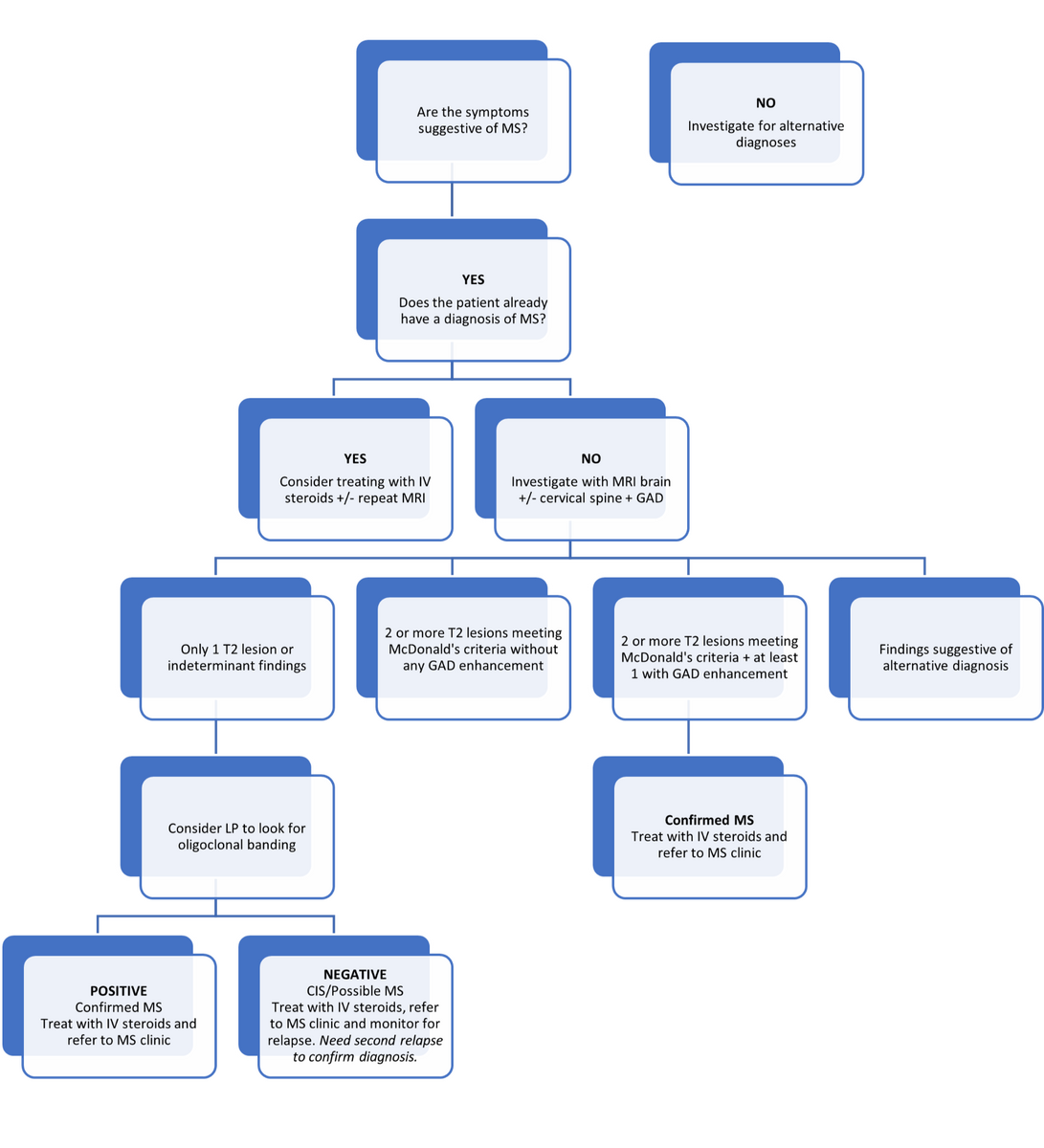
Demyelinating disease
Multiple Sclerosis
By Dr. Jane Liao
Reviewed by Dr. Alex Muccilli
Pathophysiology and Epidemiology
Chronic inflammatory disease of the CNS with evidence of demyelination and axonal damage
Mean age of onset 30 years (40 years with PPMS), affecting female : male 3:1
Risk Factors
Latitude - further from equator, greater risk; when a patient immigrates from their country of origin after 15 years old, they maintain the MS risk from the country of origin.
Low vitamin D levels and sunlight exposure
Genetics - HLA DRB1
Smoking
Adolescent obesity
Vitral triggers - EBV
For Poor Prognosis Factors for MS, see Figure 1 in this article: Reaching an evidence-based prognosis for personalized treatment of multiple sclerosis
Diagnosis of MS requires evidence of dissemination in time and dissemination in space (McDonald Criteria) through a combination of clinical and radiographic criteria
Criteria are meant to be applied to a patient presenting with symptoms consistent with CNS inflammatory demyelinating disease
NOT meant for patient with incidental MRI findings
Imperative that alternative diagnoses are considered and excluded (particularly NMO/MOG in the right contexts)
An attack/relapse/exacerbation: symptoms or signs typical of an acute inflammatory demyelinating event (current or historical) with duration at least 24 hours, in absence of fever or infection
Radiologically speaking:
Dissemination in Space (DIS): 1 or more T2 lesions in at least 2 of 4 areas (periventricular, juxtacortical, infratentorial, spinal cord)
Dissemination in Time (DIT): A new T2 and/or gadolinium enhancing lesion on follow up MRI (at least 30 days after presentation) OR simultaneous presence of asymptomatic gadolinium-enhancing and non-enhancing lesions at any time
The diagnosis can be made with:
History of 2 or more attacks and objective clinical evidence of 2 or more lesions (or objective clinical evidence of 1 lesion with reasonable historical evidence of a prior attack)
2 or more attacks but only objective clinical evidence of 1 lesion: demonstrate DIS as above or await further attack involving a different CNS site
1 attack and objective clinical evidence of 2 or more lesions: demonstrate DIT as above or await second clinical attack
1 attack and objective clinical evidence of 1 lesion (CIS): must demonstrate DIS and DIT as above or await second attack
CSF studies positive for OCBs can be used as a surrogate for DIT if the DIS criteria are met to make a diagnosis
Subtypes of MS
Clinically isolated syndrome (CIS): one clinical attack with corresponding MRI finding, but does not fit dissemination in time or space criteria
Relapsing remitting MS (RRMS): most common (80%); discrete clinical relapses with resolution of symptoms back to baseline in-between attacks
Primary progressive MS (PPMS): progression of disease from onset with variable degree of recovery; stable between episodes of PPMS
Secondary progressive MS (SPMS): initially beginning as RRMS, patients continue to have clinical attacks with less and less baseline recovery in-between attacks
Clinical features
Symptoms of MS can vary but common presentations of MS include:
Optic neuritis - reduced visual and color acuity, blurry vision, and pain with extraocular eye movements
Internuclear ophthalmoplegia - inability to adduct one eye due to lesion in MLF but with compensatory abduction Video Example
Transverse myelitis - defined sensory level loss, weakness in upper or lower extremities, autonomic dysfunction (e.g. bladder/bowel or respiratory)
Brainstem syndrome presenting with ataxia, vertigo, or dysarthria
Upper cervical cord lesions can have L'hermitte's sign (electric-like shock radiating down the back with flexion of the neck)
MS relapse usually lasts for a minimum of 24 hours without an alternative explanation. However, patients with MS can also have fluctuations in their symptoms due to concurrent infection (e.g. UTI), fevers, or heat which represent pseudo-relapses and need additional work-up
Common MS Mimics
| Inflammatory | Infectious | Neoplastic | Vascular | Metabolic/Toxic | Genetic |
|---|---|---|---|---|---|
| MOG ADEM | - | Lymphoma | Vasculitis | Osmotic myelinolysis | CADASIL |
| Neurosarcoid | Syphilis | Brain metastases | Susac’s syndrome | Carbon monoxide leukoencephalopathy | Adrenoleukodyrstrophy |
| Behcet’s | Lyme | – | Virchow-Robins spaces | Vitamin B12 deficiency | MELAS |
| Sjogren’s | HIV | – | CADASIL | PRES | Fabry’s disease |
| SLE | PML | – | – | Heroin inhalation | Familial hyperlipidemia |
| Tumefactive MS | TB | – | – | Marchiafava-Bignami disease | Phenylketonuria |
| Balo concentric rings | – | – | – | – | – |
Algorithm
Click image to enlarge
Investigations
Work-up for diagnosis
An MS diagnosis is based on clinical history and MRI. Additional investigations do NOT always need to be performed
MRI brain and spine with GAD - (important to include GAD to look for enhancing, active lesions)
Lumbar puncture - send for oligoclonobands (CSF and serum)
Bloodwork - Consider serum NMO/MOG in appropriate context
Consideration of immunotherapy
CBC, lytes, extended lytes, Cr, LFTs, TSH
Hep B core antibody, Hep C
TB skin test prior to certain immunotherapies
Strongyloides testing if from endemic region
Relapse vs pseudo-relapse
Chest x-ray, urinalysis and urine culture, blood cultures x2
Treatment
The treatment section will focus specifically on treating patients who are admitted to hospital for an exacerbation of their MS symptoms.
Glucocorticosteroids (1st line)
Indications: Acute disabling MS relapse
Dosage & Duration: IV methylprednisolone 1g OR PO prednisone 1250mg for 3-5 days
Contraindication: Sepsis or severe infection
Precautions: Administer in AM to minimize nighttime insomnia
Adverse Effects of Glucocorticosteroids
Short-term: GI upset, psychiatric symptoms (insomnia, depression, mania, hallucinations), hyperglycemia, susceptibility to infections
Long-term: Hypertension, weight gain, osteoporosis and avascular necrosis of the hip (rare)
Plasma Exchange (2nd line)
No clear evidence for PLEX in people with MS, though sometimes used in an off-label fashion if severe relapse with poor recovery
Indications: Acute, severe MS relapses poorly responsive to glucocorticosteroids
Dosage & Duration: 1 PV exchange x7 over 14 days
Contraindications: Prior anaphylactic reaction
Precautions: Central line insertion may be required
Adverse Effects of Plasma Exchange
Mild: Citrate toxicity, hypotension, fever/chills/rigor, urticaria, pruritis
Severe: Arrythmia, thromboembolism, pulmonary edema, seizures, coagulopathy, angioedema, bronchospasm, anaphylaxis
Indications: Acute, severe MS relapses poorly responsive to glucocorticosteroids or PLEX; MS relapses in pregnancy
Dosage & Duration: 2 g/kg over 2-5 days
Contraindication: Prior anaphylactic reaction
Neuromyelitis Optica Spectrum Disease (NMOSD)
By Dr. Andrea Kuczynski
Reviewed by Dr. Alex Muccilli
Pathophysiology and Epidemiology
NMOSD is an inflammatory disease of CNS characterized by episodes of optic neuritis, transverse myelitis, and other focal neurological symptoms
AQP4 (Aquaporin-4) IgG is the most common antibody found in patients with NMOSD (80% of cases)
Consider MOG (myelin oligodendrocyte glycoprotein) IgG in seronegative patients
Less common in predominantly Caucasian countries
Diagnostic Criteria of NMO with (+) AQP4 IgG:
One core clinical feature: optic neuritis, acute myelitis, area postrema syndrome, other brainstem syndrome, symptomatic narcolepsy or acute diencephalic syndrome with with MRI lesion(s), symptomatic cerebral syndrome with MRI lesion(s)
No better explanation
Diagnostic Criteria of NMO without AQP4 IgG:
2+ core clinical features including 1 of optic neuritis, acute myelitis, or area postrema syndrome
Meets MRI requirements for clinical features (see below)
Dissemination in space met with two or more different core clinical characteristics
No better explanation for the clinical syndrome
Negative testing for AQP4 IgG (ideally with cell-based testing)
MRI criteria for seronegative NMOSD
Optic neuritis with either normal MRI or optic nerve lesion (T2/FLAIR or T1-GAD) involving more than half of the optic nerve or chiasm
Acute myelitis with MRI cord lesions extending over 3 + continuous segments (or atrophy in patients with remote history of myelitis)
Acute area postrema syndrome: Dorsal medulla lesion
Acute brainstem syndrome: Periependymal brainstem lesions
| MS | NMO | MOG | |
|---|---|---|---|
| Optic neuritis | Variable severity (rarely severe) with 2/3 affecting posterior optic nerve, good recovery | Can present as bilateral simultaneous optic neuritis; posterior nerve involvement and may involve optic chiasm; uncommon to have disc edema; more severe with poor prognosis for visual recovery (; can have recurrent attacks | Can present as bilateral simultaneous or unilateral optic neuritis; longitudinal, anterior optic neuritis; disc edema and perineural gadolinium enhancement; better visual outcome than NMO |
| Transverse myelitis | Preference for posterior and lateral cord; lesions will be less than 3 vertebral bodies in length | Lesion extends 3+ vertebral segments; preference for central cord but can expand; more than ⅔ of the axial cord will be involved swollen cord; enhancement; often poor prognosis with permanent gait instability | Linear or expansile lesions, preference for conus |
Investigations
Serum anti-aquaporin-4 IgG - greater specificity than in CSF and with cell based assays
Serum MOG antibodies - greater specificity than in CSF
Do not test MOG in all patients with MS; only send off antibodies in appropriate clinical scenarios
MRI brain +/- spine (depending on symptomatology)
Lumbar puncture if indicated to rule out other causes of optic neuritis/transverse myelitis as indicated
Treatment
Acute therapy: pulse steroids, early PLEX if disabling symptoms (see MS section)
Maintenance: MMF, Rituximab, Azathioprine
New agents that can be used: Eculizumab, Satralizumab, Inebilizumab for AQP4+ NMOSD
MOG+ disease may require longterm immunosuppression with agents such as MMF, Azathioprine, Rituximab, or monthly IVIG
Patient Education
Pediatric patients with ADEM have a 10-15% risk of developing or initially presenting with MOG
Many cases of MOG are monophasic
AQP4+ NMO can be paraneoplastic so consider screening for malignancy in elderly individuals
MOG and MS have typically better functional recovery than NMO
Transverse Myelitis
By Dr. Andrea Kuczynski
Definitions
Transverse myelitis: heterogeneous group of disorders with acute to subacute inflammatory spinal cord syndrome
“Complete” cord lesion: relatively symmetric moderate or severe sensory-motor loss. Suggestive of a monophasic disorder (i.e., infectious) or relapsing NMO
“Partial” cord lesion: incomplete or patchy involvement of at least one spinal segment with mild to moderate weakness and asymmetric or dissociated sensory symptoms. More likely secondary to MS with high risk for relapses in the future
Diagnostic Criteria of Transverse Myelitis
Development of sensory, motor, or autonomic dysfunction due to spinal cord etiology
Clearly defined sensory level
MRI-confirmed exclusion of extra-axial compressive etiology
Inflammation within the spinal cord - CSF pleocytosis, elevated IgG index, or gadolinium enhancement
Progression to nadir between 4 hours and 21 days following symptom onset
Differential Diagnosis
| Demyelinating | Infectious | Inflammatory | Neoplastic | Metabolic | Vascular |
|---|---|---|---|---|---|
| MS | VDRL | Sarcoidosis | CNS lymphoma | Vitamin B12 | Dural AV fistula |
| NMO | Viral (WNV, Polio, HSV2, EBV, CMV) | SLE | Ependymoma | Vitamin E | - |
| MOGAD | TB | Sjogren’s | Astrocytoma | Copper | - |
| ADEM | Lyme | Scleroderma | Paraneoplastic syndrome (anti-Hu, anti-CRMP-5) | - | - |
| - | HIV | Behcet’s | Primary intramedullary tumor | - | - |
| - | HTLV-1 | - | - | - | - |
Clinical Features
Bowel/bladder dysfunction - constipation, urinary retention, urinary/fecal incontinence
Weakness - upper and/or lower limb involvement depending on spinal level
Hypotonia in affected limbs
Numbness, paraesthesias - upper and/or lower limb involvement depending on spinal level
Pain or tightness - often occurring around stomach or chest
+/- Lhermitte sign
Paroxysmal tonic spasms
Investigations
CT lumbar spine if bowel/bladder symptoms - first rule out cauda equina and indication for surgery!
MRI spine with contrast (level depends on limb involvement)
Serum NMOSD antibodies (see NMOSD section)
LP including infectious work-up
Rheumatological work-up: ANA, anti-dsDNA, ENA, RF, ANCA, C3/C4, APLA
HIV, VDRL, Lyme serology
Vitamin B12, vitamin E
Serum copper
Treatment
Solumedrol 1g IV daily x5 days then maintenance Prednisone 1 mg/kg with slow taper
IVIG 2 g/kg IV over 2 days if no response to steroids
PLEX
Prophylaxis while on high dose steroids: calcium, vitamin D, PPI, PJP prophylaxis
Management of comorbid symptoms (i.e., neuropathic pain, bowel regimen, spasticity, spasms)
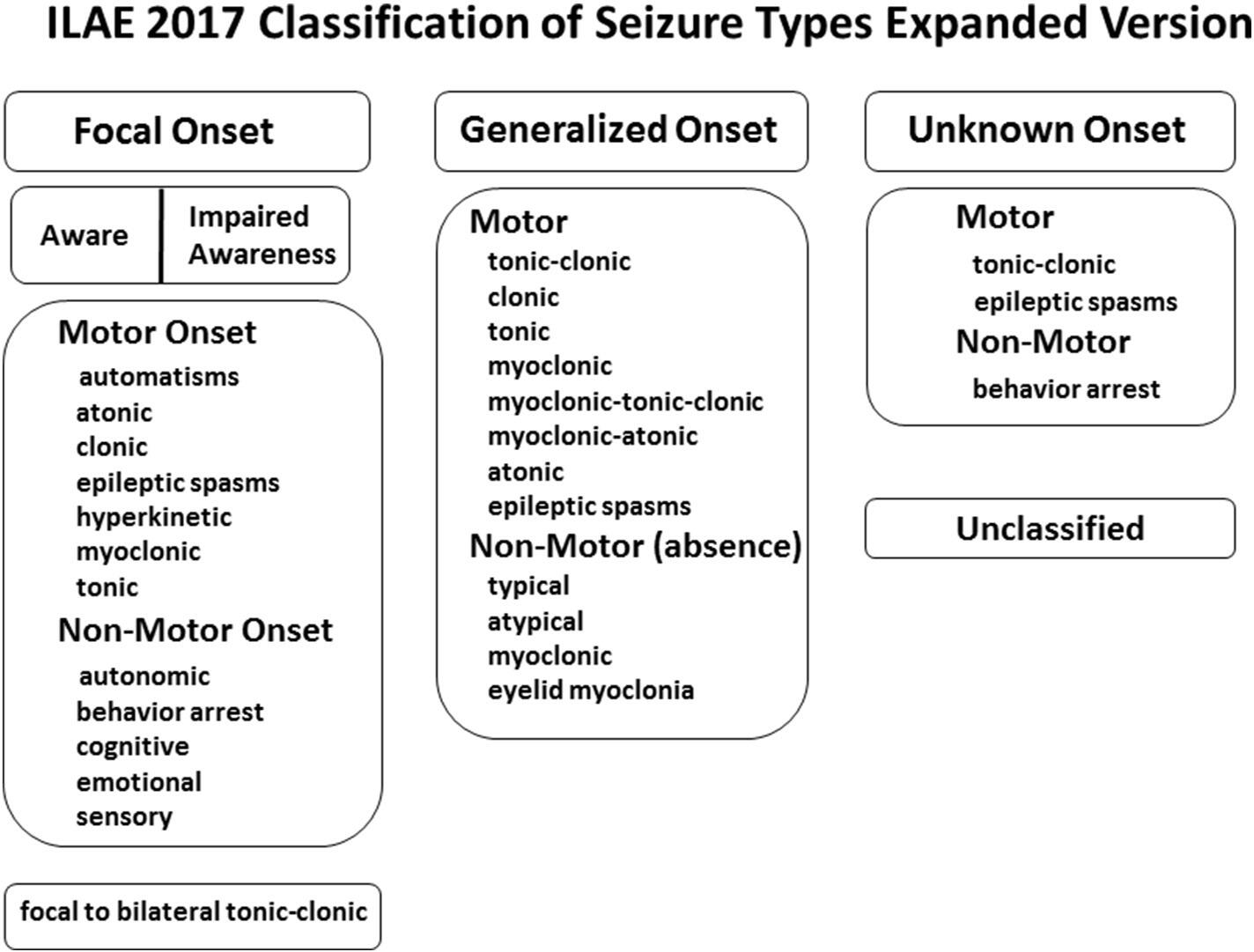
Seizure
Seizure
By Dr. Andrea Kuczynski
Reviewed by Dr. Jerry Chen and Dr. Matthew Burke
Definition
Seizure: A transient occurrence of signs and/or symptoms (e.g. sensory, motor, speech, consciousness) due to abnormal excessive or synchronous neuronal activity in the brain
Epilepsy: disorder of the brain with an enduring predisposition to generate epileptic seizures and by the neurobiological, cognitive, psychological, and social consequences of this condition; in a patient who has any of the following:
1) at least 2 unprovoked seizures occurring >24 hours apart;
2) one unprovoked (or reflex) seizure and a probability of further seizures (similar to the general recurrence risk after two unprovoked seizures (at least 60%) occurring over the next 10 years (e.g. abnormal imaging with a potential seizure focus or EEG with epileptiform activity);
3) diagnosis of epilepsy syndrome (e.g. West, Dravet, Lennox-Gastaut)
Provoked seizure: occur with an identifiable proximate cause (metabolic, toxic, structural, infectious, inflammatory) and are not expected to recur in the absence of that particular cause/trigger (e.g., hypoglycemia, alcohol withdrawal, etc.)
Unprovoked seizure: occur without an identifiable cause or in the context of a remote symptomatic cause (i.e., pre-existing brain lesions, such as a remote stroke). Recurrent unprovoked seizures are more likely to be associated epilepsy
Focal onset (“partial”) seizure: abnormal synchronous neuronal activity originating from one location (within limited to one hemisphere) of the brain, more concerning to be associated with elevated future recurrence risk
Generalized onset seizure: abnormal synchronous neuronal activity arising within and rapidly engaging bilaterally distributed networks
Click image to enlarge
Differential Diagnosis
Stroke/TIA
Syncope: cardiac arrhythmia, orthostatic syncope, vasovagal syncope
Migraine
Encephalopathy: drug-induced, metabolic disturbance
Psychiatric: anxiety/panic attack, PNES
| TIA | Seizure | Migraine Aura | |
|---|---|---|---|
| Etiology | Vascular risk factors (e.g. CAD, atherosclerosis) | Trauma, brain lesions (e.g. previous strokes, tumors) | Migraines |
| Cardiovascular manifestations | Frequent | N/A | N/A |
| Neurological manifestations* | Negative symptoms (deficits - weakness, vision loss) | Positive symptoms but can have negative symptoms post-ictal (Todd's Paresis) | Positive symptoms (visual more common), headaches |
| Symptom onset | Sudden | Less than 2 minutes with progression | More than 10 minutes with progression |
| Duration | 5-10 minutes | Less than 5 minutes | More than 20 minutes |
Psychogenic Non-epileptiform seizures (PNES)
Involuntary events in response to internal or external triggers that have similar features to those seen in epileptic seizures, but without corresponding electrophysiological features (i.e., epileptiform discharges)
Patients with epilepsy can also have PNES
Associated with adverse events and trauma
Triggers for PNES may include positional change, physical exertion, emotional/stressful situations, dehydration, or heat
Treatment may involve education and support (see Functional Neurological Disorders section)
| PNES | Epileptic Seizure | |
|---|---|---|
| Preceding aura | Can be variable with shorter duration over time due to dissociation | Sensory, experiential (e.g., déjà vu, jamais vu), autonomic aura |
| Onset of myoclonus | Follows loss of consciousness, occurs with situational associations and often has preserved awareness | Immediate |
| Eye deviation | Upward, often with closed eyes and resistance to eyelid opening | Lateral, with eyes open |
| Myoclonus rhythm | Arrhythmic jerks | Rhythmic jerks |
| Myoclonus pattern | Multifocal jerks briefly involving bilateral proximal and distal muscles; may see pelvic jerking | Unilateral or asymmetric jerks, may exhibit neuroanatomic evolution or GTC behaviour |
| Post-ictal presentation | Fatigue but no confusion, with relatively rapid recovery to baseline | Confusion, +/- Todd’s paresis (hemiparesis) |
Risk factors
Traumatic brain injury
Abnormalities in childhood development and birth history
Febrile seizures
Meningitis and/or untreated meningitis
Intracranial structural lesion: (gliosis, encephalomalacia, mass lesion, developmental malformations, cavernomas)
Previous seizure/epilepsy history
Family history
Neurodegenerative disorders
Seizure triggers
Sleep deprivation
Substance use/withdrawal
Infection
Trauma
Menstruation and ovulation
Non-adherence to treatment
Metabolic abnormalities: hypoglycemia, hyponatremia >hypernatremia, hypocalcemia > hypercalcemia, hypomagnesium
Clinical Features
Preceding aura: somatosensory, experiential (i.e., deja vu, jamais vu, epigastric rising sensation), motor, speech/language, autonomic, olfactory/gustatory, and/or visual perceptual disturbance experienced prior to the seizure with positive phenomenology
Event: level of awareness, circumstances leading up to the event (i.e., sleeping, awake), duration, movements (i.e., facial movements, head deviation, eye movements and deviation, rhythmic vs. arrhythmic limb movements, tonic clonic, posturing), urinary/fecal incontinence, tongue biting
Post-ictal period: confusion, drowsiness/altered level of consciousness, Todd’s paresis (hemiparesis), duration to return to baseline; important to complete neurological examination following event and assess for lateralizing signs
Investigations
Stat CT head to rule out acute intracranial abnormality (i.e., hemorrhage, stroke, mass lesion)
CBC
Lytes, extended lytes (Mg, Ca, PO4), creatinine
Blood glucose
CK
Prolactin (When considering PNES, should be drawn within 10-20 minutes, should be ~2x versus baseline)
Liver enzymes
Toxicology screen if indicated
Blood, urine, CSF cultures if indicated
MRI brain with contrast (seizure protocol) when clinically stable: may see some T2/FLAIR hyperintensity, diffusion restriction (ADC drop >10% is associated with permanent damage)
EEG
AED levels if prescribed to patient
LP with cell count and differential, protein, glucose, bacterial/viral/fungal cultures, cytology/flow cytometry, autoimmune/paraneoplastic panels as indicated
Serum autoimmune/paraneoplastic panels if indicated
Autoimmune work-up: ANA, anti-dsDNA, ENA, RF, C3/C4, cryoglobulins as indicated
If there is suspicion for PNES - prolonged video EEG or EMU is helpful for the diagnosis
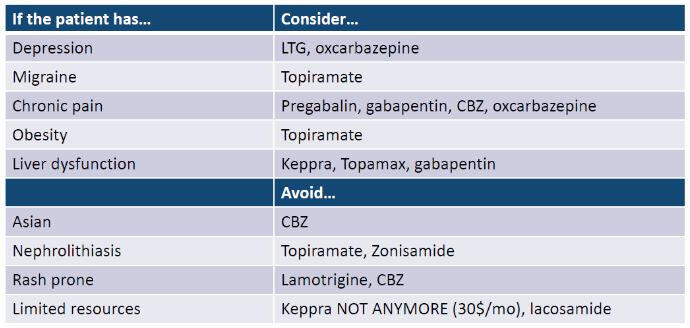
Treatment
ABCs (airway, breathing, circulation) and consultation of ICU if the patient may require intubation with prolonged seizure
First-line Benzodiazepines - Midazolam 10mg IM x1 (if patient is >40kg) or Lorazepam 2mg IV q2min (max 8mg)
AED load after acute management if indicated
Patients with a single provoked seizure do not typically require maintenance AED
Maintenance AED: predominantly used if unprovoked seizure with high risk of recurrence or multiple unprovoked seizures or abnormal EEG/MRI or nocturnal seizures
If suspicious of infectious cause, antimicrobials based on suspected organism/etiology should be initiated after the collection of cultures (if possible)
Correction of metabolic abnormalities
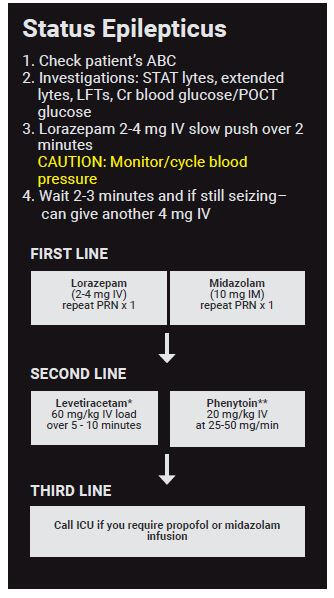
For Pocket Card Algorithm in Status Epilepticus, see Figure 1 in this article: The Efficacy and Use of a Pocket Card Algorithm in Status Epilepticus Treatment
| AED | Load Dose and Rate | Maintenance Dose | Clearance | Side-effects for Monitoring |
|---|---|---|---|---|
| Phenytoin | 20 mg/kg IV at a rate no faster than 50 mg/min | Start at 300mg p.o. Daily (up to 400mg BID) | Hepatic | Cardiac side-effects (hypotension, QTc prolongation), avoid if possible in patients with hepatic dysfunction |
| Keppra | 40-60 mg/kg IV (max 4500mg) over 5-10 min | Start at 500mg p.o. BID (up to 1500mg BID) | Renal | Avoid if possible in patients with anxiety/depression or renal dysfunction |
| VPA | 20-40 mg/kg IV (max 3000mg) over 20 min | Start at 500mg p.o. BID (up to 750mg BID) | Hepatic | May affect platelet function even without thrombocytopenia, Avoid if possible in patients with hepatic dysfunction |
| Lacosamide | 200-400mg IV | Start at 100mg IV/p.o. BID (up to 200mg BID) | Renal more than hepatic | Cardiac side-effects (PR interval prolongation, heart block, bradycardia), Avoid in patients with type 2 or 3 heart block, sick sinus syndrome |
Click image to enlarge
[Source: Dr. Arina Bingeliene's Emergency Lecture 2020]
In choosing a long-term AED, consider the following:
Seizure type (focal vs. generalized onset, specific seizure syndrome)
Comorbidities
Side effects and tolerance
Dosing frequency
Drug coverage/affordability
Teratogenic AEDs to avoid in pregnancy:
VPA
Carbamazepine
Topiramate
Phenytoin
Phenobarbital
OCP efficacy is reduced by:
High Topiramate levels
Enzyme inducers: Phenytoin, Carbamazepine
Phenobarbital, primidone, oxcarbazepine
Patient Education
Driving: reporting to MTO is a mandatory obligation in Ontario and instruct the patient not to drive until driving privileges are reinstated by the MTO
Precautions to counsel patients surrounding baths alone, swimming alone, heights/dangerous activities (e.g. climbing ladders)
Status Epilepticus
By Dr. Andrea Kuczynski
Reviewed by Dr. Alex Muccilli
Definition
A single seizure lasting more than 5 minutes or multiple seizures with incomplete recovery of level of consciousness to baseline between the seizures
May present as generalized tonic clonic (GTC) seizures or non-convulsive seizures
Defined by 2 time-points: T1 (time beyond which seizures will likely prolong >5 minutes GTC) and T2 (GTC 30 minutes with higher risk for long-term consequences)
Mortality is 20% - most important determinant of mortality is underlying cause
Evidence supporting early treatment of seizures stems from studies showing increasing pharmaco-resistance (especially to benzos) and neuronal injury with longer seizure durations
Causes of status epilepticus
Neuroleptic Malignant Syndrome
Serotonin Syndrome
Substance use/withdrawal
Autoimmune encephalitis - suspect if no response to AEDs
Clinical Features
GTC seizure with head and gaze deviation, +/- urinary/fecal incontinence
Non-convulsive seizure - nystagmus, sustained eye deviation, facial/periorbital twitching, abnormalities in vital signs
Post-ictal phenomenon - confusion/agitation, dysarthria/aphasia, altered level of consciousness, Todd’s paresis (unilateral hemiparesis)
Investigations
Stat CT head to rule out acute intracranial abnormality (i.e., hemorrhage, stroke, mass lesion)
CBC
Lytes, extended lytes (Mg, Ca, PO4), creatinine
Blood glucose
Liver enzymes
Toxicology screen if indicated
Blood, urine, CSF cultures if indicated
MRI brain with contrast (seizure protocol) when clinically stable: may see some T2/FLAIR hyperintensity, diffusion restriction (involving cortex, hippocampi/mesial temporal lobes, thalamus, and cerebellum)
EEG
AED levels if prescribed to patient
LP with cell count and differential, protein, glucose, bacterial/viral/fungal cultures, cytology/flow cytometry, oligoclonal bands/IgG index, autoimmune/paraneoplastic panels as indicated
Serum autoimmune/paraneoplastic panels if indicated (see requistions)
Treatment
ABCs (airway, breathing, circulation) and consultation of ICU as the patient may require intubation with prolonged seizure
First-line Benzodiazepines - Midazolam 10mg IM x1 (if patient is >40kg) or Lorazepam 2mg IV q2min (max 8mg)
AED load after acute management
| AEDS | Dose and Rate | Side-effects for Monitoring |
|---|---|---|
| Phenytoin | 20 mg/kg IV at a rate no faster than 50 mg/min | Cardiac side-effects (hypotension, QTc prolongation), Purple Glove Syndrome (Extensive skin necrosis and limb ischemia), Avoid if possible in patients with hepatic dysfunction |
| Keppra | 40-60 mg/kg IV (max 4500mg) over 5-10 min | Avoid if possible in patients with anxiety/depression or renal dysfunction or dose accordingly |
| VPA | 20-40 mg/kg IV (max 3000mg) over 20 min | May affect platelet function even without thrombocytopenia, hyperammonemia, pancreatitis, Avoid if possible in patients with hepatic dysfunction |
| Lacosamide | 200-400mg IV bolus then 100mg IV BID | Cardiac side-effects (PR interval prolongation, heart block, bradycardia), Avoid in patients with type 2 or 3 heart block, sick sinus syndrome |
* Max dose of Levetiracetam is 4.5 g for status epilepticus
** In an average-size (70 kg) individual, consider 1500 mg load of
phenytoin if unable to obtain weight quickly
Click image to enlarge
Consider giving thiamine 500 mg IV followed by 50 ml of D50
Intubated patients may require burst suppression (target 40-60%) and ICU monitoring with titration of sedatives including propofol and barbiturates
If suspicious of infectious cause, antimicrobials based on suspected organism/etiology should be initiated after the collection of cultures (if possible)
Correction of metabolic abnormalities
* Max dose of Levetiracetam is 4.5 g for status epilepticus
** In an average-size (70 kg) individual, consider 1500 mg load of
phenytoin if unable to obtain weight quickly
Patient Education
For patients with known seizure disorders, compliance to AEDs is important to reduce risk of status epilepticus
Movement disorders
Parkinson's Disease (PD)
By Dr. Priti Gros
Reviewed by Dr. Emily Swinkin
Pathophysiology and Epidemiology
Second most common neurodegenerative disorder following Alzheimer's disease
Due to dopamine deficiency secondary to degradation of dopaminergic neurons in the substantia nigra
Can be genetic (10%) or idiopathic (90%)
Average age of onset in 60’s
Pathologically characterized as an alpha synuclein proteinopathy with presence of Lewy bodies
Clinical Features
Cardinal features of Parkinsonism are: 4-6 Hz Rest tremor, Rigidity, Akinesia/Bradykinesia, and Postural instability not due to visual, vestibular, or cerebellar or proprioceptive dysfunction (TRAP)
Non-motor features of PD: Rapid eye movement (REM) sleep disorders, anosmia, autonomic dysfunction (constipation, orthostatic hypotension), mood changes, cognitive changes
Constipation, REM sleep disorders, and anosmia can precede motor symptoms of PD by over a decade
At present there are no confirmatory diagnostic tests for PD, it is a clinical diagnosis
Many diseases have Parkinsonism features - important to distinguish from PD as they often do not respond to levodopa. Examples include the following:
Drug induced: Antipsychotic use (especially first generation like haloperidol) and dopamine antagonists (e.g. metoclopramide) - can often have tardive dyskinesia and akathsias
Toxins: Manganese, MPTP
Vascular parkinsonism: concomitant vascular risk factors, may be more symmetric and have lower body predominance
Parkinson’s Plus Syndromes (see below)
| Etiology | PSP | MSA | CBS | DLB |
|---|---|---|---|---|
| Age of onset | 60’s | 50’s | 60’s | 50-80’s |
| Features | Difficulties with vertical gaze, falls, axial rigidity | Autonomic dysfunction, cerebellar signs, upper motor neuron signs | Alien limb, apraxia, myoclonus, cortical signs and cognitive impairment | Cognitive changes progressing to dementia with visual hallucinations onset BEFORE or shortly after parkinsonism |
| Neuroimaging | Humming bird and Mickey Mouse sign | Hot cross bun sign | Asymmetrical parietal/basal ganglia atrophy | N/A |
Diagnosis
UK Parkinson’s Disease Society Brain Bank Criteria:
Step 1: Diagnosis of parkinsonism requires bradykinesia and one of the following features:
Rigidity
4-6 Hz rest tremor
Postural instability “not caused by primary, visual, vestibular, cerebellar or proprioceptive dysfunction
Step 2: Exclusion of “red flags”. One or more could suggest another diagnosis (e.g. Parkinson’s Plus Syndromes)
History of repeated strokes with stepwise progression of parkinsonism
History of repeated injury
History of definitive encephalitis
Neuroleptic treatment at onset of symptoms
MPTP exposure
Negative response to large doses of levodopa
>1 relative affected (this criteria is usually no longer applied)
Sustained remission
Strictly unilateral features after 3 years
Early severe autonomic involvement
Early severe dementia with disturbances of memory, language and praxis
Oculogyric crises
Supranuclear gaze palsy
Babinski sign
Cerebellar signs
Presence of cerebral tumor or communicating hydrocephalus on CT or MRI
Step 3: Supportive features for PD. 3 or more are required for diagnosis of definite PD:
Unilateral onset
Rest tremor
Progressive disorder
Persistent asymmetry affecting the side of onset most
Excellent response (70-100%) to levodopa
Severe levodopa-induced chorea
Levodopa response for 5 years or more
Clinical course of 10 years or more
Physical Exam
Key exam maneuvers and features in Parkinson’s Disease or Parkinson’s Plus Syndromes
Inspection: Decreased facial expression (hypomimia), softer voice (hypophonia), decreased blink rate
Eye movements: Difficulties with extraocular eye movements (e.g. PSP - slowed or impaired vertical saccades), hypometric saccades (Can be tested with OKN strips, in PSP - decreased vertical saccades)
Tremor: Parkinson’s tremor typically occurs at rest and is asymmetrical, but can re-emerge with sustained posture, often described to have a “pill-rolling” quality and can worsen with distraction (“Count months of the years backwards”)
Bradykinesia: Finger tapping, hand open-close, supination-pronation, foot and heel tapping will demonstrate not just slowness but decrement in amplitude or freezing of movements
Tone: Testing for both appendicular rigidity (usually Parkinson’s Disease) and axial rigidity (often seen in PSP)
Gait: Slow, shuffling gait with often stooped posture. Arm swing can be diminished with emergence of tremor. Difficulty with turns, requiring multiple steps to move (en-bloc turning). Patients can walk slowly but then accelerate with small steps (festination). Advanced PD can demonstrate freezing of gait at times which are overcome by visual stimuli (e.g. stepping over a line)
Postural instability: Pull test to look for retropulsion (will require several >3 steps to regain balance)
Other signs: Micrographia or tremor in writing
Investigations
Atypical symptoms may benefit from MRI brain to rule out Parkinson’s Plus syndromes
Treatment
No disease-modifying therapy, only symptomatic management is available yet (see below):
Symptomatic management of motor PD symptoms
| Class of medications | Levodopa | Dopamine agonists | Monoamine oxidase type B inhibitors (MAO-B) | COMT-inhibitors | Anticholinergic drugs |
|---|---|---|---|---|---|
| Medications | Levodopa-Carbidopa (Sinemet) | Pramipexole, Ropinirole, Rotigotine | Selegiline, Rasagiline, Safinamide | Entacapone | Trihexylphenidyl |
| Indications | Usually first line, start at Sinemet 100/25 1 tab TID, must be taken with food and protein can reduce efficacy | Less well tolerated in elderly patients due to confusion but less incidence of fluctuations and dyskinesia | Usually add-on to improve efficacy of levodopa | Usually add-on to improve efficacy of levodopa | Best for tremor predominant but only for younger individuals |
| Side Effects | Nausea, GI upset, daytime somnolence, orthostatic hypotension, oedema and can induce dyskinesia in long-term | Nausea, daytime somnolence, hallucinations, impulse control disorders (pathological gambling, hypersexuality, binge eating). | Theoretical risk of serotonin syndrome if on an SSRI/SNRI | Confusion, hallucination, urine discolorations, diarrhea, and dyskinesias | NOT FOR ELDERY, dry mouth, constipation, somnolence, memory changes |
Treatment of non-motor Parkinson's Disease symptoms (non-exhaustive list)
Depression: Dopamine agonist (Pramipexole), Serotonin reuptake inhibitor (Citalopram, Fluoxetine), Serotonin and Norepinephrine Reuptake Inhibitor (Venlafaxine), Tricyclic antidepressant (Desipramine, Nortriptyline),
Psychosis: Atypical antipsychotic (Clozapine, Quetiapine), acetylcholinesterase inhibitor (Rivastigmine)
REM Sleep behaviour disorder: Hormone (Melatonin), Benzodiazepine (Clonazepam)
Constipation : Osmotic laxative (PEG)
Gastrointestinal motility : Peripheral dopamine antagonist (Domperidone)
Orthostatic hypotension: peripheral dopamine antagonist (Domperidone), Mineralocorticoid (Fludrocortisone), Vasopressor (Midodrine)
Essential Tremor
By Dr. Priti Gros
Reviewed by Dr. Emily Swinkin
Epidemiology
Common, can be both familial (about 50% will have a family history although no single causative gene yet identified) or idiopathic
Two peaks of onset at 20s and 60s
Clinical Features
Usually an isolated tremor syndrome of the bilateral upper limb presenting as a posture or kinetic tremor, with or without head tremor or tremor in other locations
Benign, but tremors can become progressively worse which may warrant symptomatic treatment
Tremors may improve with small amounts of alcohol
Diagnostic criteria: Essential Tremor
Isolated tremor syndrome of bilateral upper limb action tremor
At least 3 years’ duration
With or without tremor in other locations (e.g. head, voice or lower limbs)
Absence of other neurological signs, such as dystonia, ataxia, or parkinsonism
Exclusion criteria for ET
Isolated focal tremors (voice, head)
Orthostatic tremor with a frequency > 12 Hz
Task- and position-specific tremors
Sudden onset and step-wise deterioriation
Differential Diagnosis
Enhanced physiological tremor: common bilateral upper limb action tremor (8-12 hz), caused by anxiety, fatigue, hyperthyroidism, other drugs. It is often reversible if the cause of the tremor is removed
Parkinson’s disease and other forms of Parkinsonism: classic parkinsonian tremor is typically a 4-7 Hz rest tremor. It can involve the upper or lower extremities, jaw or tongue. See section on Parkinson’s disease. See section on Parkinson’s disease
Cervical dystonia: common cause of isolated head tremor.
Task- and position-specific tremors: focal tremor that typically occur during a specific task or posture
Primary orthostatic tremor: a generalized high frequency (13-18 hz) isolated tremor syndrome that occurs upon standing up. Often, confirmation of the tremor frequency is done using electromyography
Functional tremor: characterized by distractibility, frequency entrainment or antagonistic muscle coactivation
Investigations
Generally no investigations are needed unless there are atypical findings
Treatment
First line treatments
Propranolol
Initial dose: 60 - 80 mg/day (divided into two or three doses per day, e.g. 40 mg BID) and gradually titrate up to efficacy (may start at lower dose in elderly)
Maintenance dose : 120 to 320 mg/day (Lower dose is better for elderly individuals)
Side Effects: Lightheadedness, bradycardia, fatigue
Contraindications: Patients with heart block/heart failure, asthma, and type 1 diabetes
Primidone
Initial dose: 25 mg/day (at bedtime) and increase by 25 mg every 3-7 days
Maintenance dose : 250 mg - 500 mg/day
Side Effects: Sedation, drowsiness, fatigue, nausea and vomiting, ataxia
Second line treatments
Propranolol + Primidone
Gabapentin 100-300mg p.o. TID (max 1200mg daily)
Topiramate 25mg p.o. daily-BID (max 400mg daily)
Surgical treatments
MRI-guided focused ultrasound thalamotomy
Deep brain stimulation to thalamus
Patient Education
The clinical course of ET is typically slow, progressive over years
Younger age of onset usually correlates with slower progression
Myoclonus
By Dr. Caz Zhu
Reviewed by Dr. Emily Swinkin
Definition
Sudden, brief involuntary muscle jerks that occur occur at rest, movement, or provoked by stimuli (e.g. touch, sound)
Positive myoclonus: Caused by abrupt muscle contraction
Negative myoclonus: Caused by loss of tone (e.g. asterixis)
Clinical Features
Cortical myoclonus: Usually affecting the face and hands and with voluntary action. stimulus sensitive and triggered by action or touch, can also be seen in certain epilepsy syndromes
Subcortical/Brainstem myoclonus: Generalized jerks in axial and bilateral proximal extremities, stimulus sensitive to auditory triggers - startle response (e.g. loud clap)
Spinal myoclonus (Propriospinal myoclonus and segmental spinal myoclonus): Usually arrhythmic jerks in the arm/trunk but in propriospinal myoclonus, you can see abdominal myoclonus (torso flexion)
Secondary myoclonus is the most common form of myoclonus - due to an underlying neurological or non-neurological cause → important to differentiate whether onset of myoclonus is acute vs gradual
Diffuse myoclonus is often seen post-anoxic brain injury (associated with poor prognosis) - e.g. Lance-Adams Syndrome
Differential Diagnosis
*This is not an exhaustive list but some of the common causes of myoclonus to consider
| Classification | Common causes |
|---|---|
| Toxic-Metabolic | Hepatic & renal failure, electrolyte abnormality, hyperthyroidism |
| Drug-induced | SSRIs, dopamine agonists, opioids, antibiotics (cephalosporins), benzodiazepine withdrawal |
| **Infectious ** | Herpes Simplex Encephalitis |
| Trauma | Lance-Adams Syndrome (action-induced myoclonus during recovery of anoxic brain injury) , spinal cord injury |
| Neurodegenerative Diseases | CJD, cortico-basal degeneration, other dementias |
| Paraneoplastic | Anti-Ri antibodies (breast and lung cancer) |
| **Epileptic Myoclonus ** | Childhood myoclonic epilepsy (lennox-gastaut syndrome), Progressive myoclonus epilepsy (MERRF) |
| Essential | Purely isolated myoclonus |
| **Physiological ** | Hynagogic myoclonus (falling asleep), hiccups, physiological startle |
Investigations
CBC, lytes, extended lytes, LFTs, TSH
MRI brain in appropriate clinic context to evaluate for anoxic injury, brainstem pathology, neurodegenerative conditions
EEG and EMG may be helpful but generally not required for diagnosis
Treatment
If reversible cause of myoclonus is found (e.g. due to metabolic cause or drug-induced) - need to treat
Symptomatic treatment for myoclonus:
| Cortical | Subcortical | Spinal | Focal peripheral myoclonus (hemifacial spasm) | |
|---|---|---|---|---|
| Therapies | Valproic acid, Clonazepam, and Levetiracetam | Clonazepam | Clonazepam | Botox injections |
Stroke
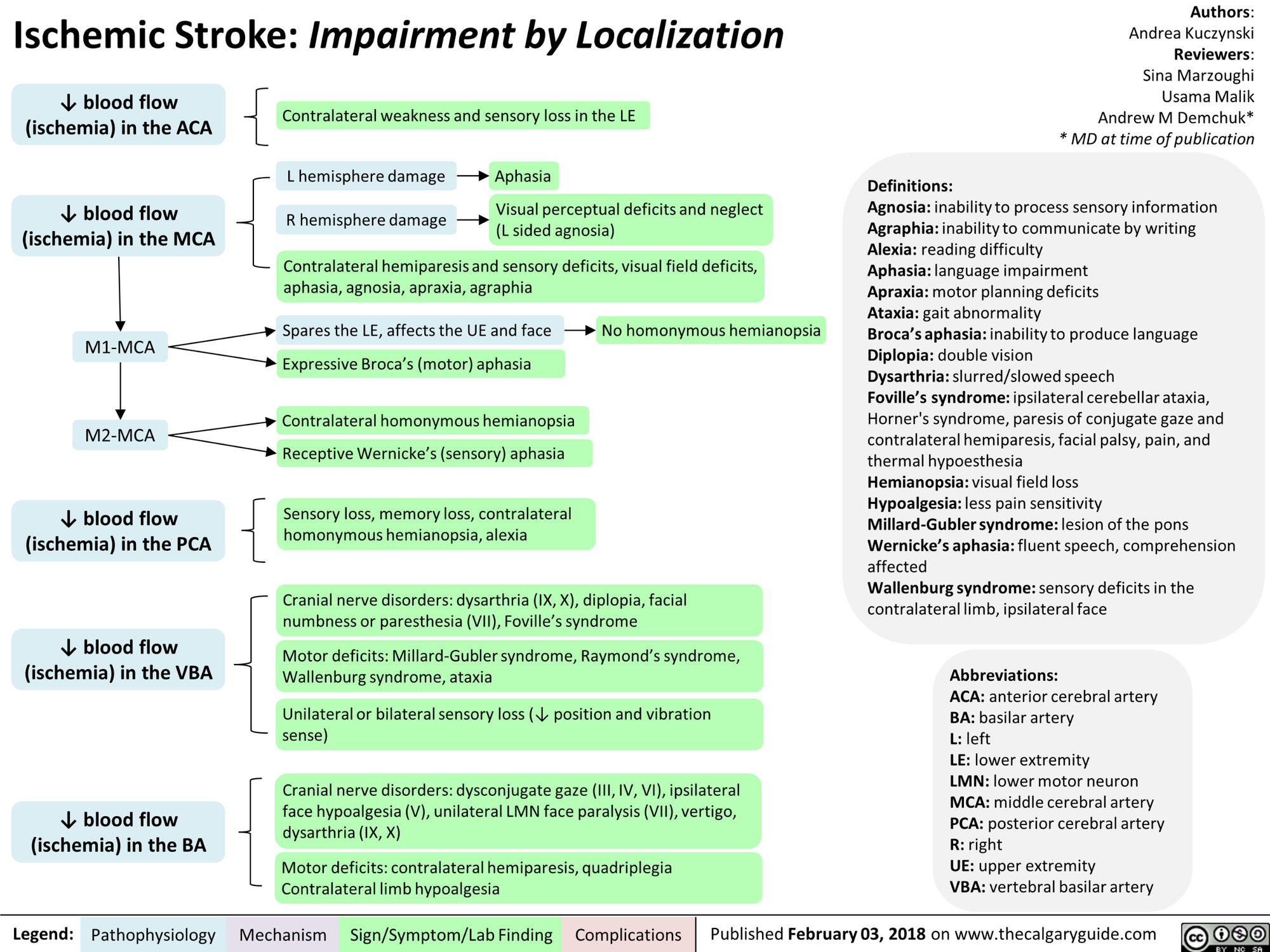
Ischemic Stroke
By Dr. Andrea Kuczynski
Reviewed by Dr. Houman Khosravani
Definitions
Ischemic stroke: hypoperfusion of brain tissue due to thrombus/embolus within the intracranial vasculature
TIA*: transient episode of neurological dysfunction due to focal ischemia without infarction; should see resolution of symptoms without neuroimaging correlate if symptoms resolve within 24hrs and typically do not see neuroimaging correlate if symptoms resolve within 2hrs
High risk TIA: high risk for occurrence of an ischemic stroke within the first 48hrs in a patient with transient unilateral motor and/or speech/language symptoms lasting >5 minutes
Increasingly, there is recognition that TIA is not the best terminology and we expect the field to revolve to potentially remove this term; but for now it remains
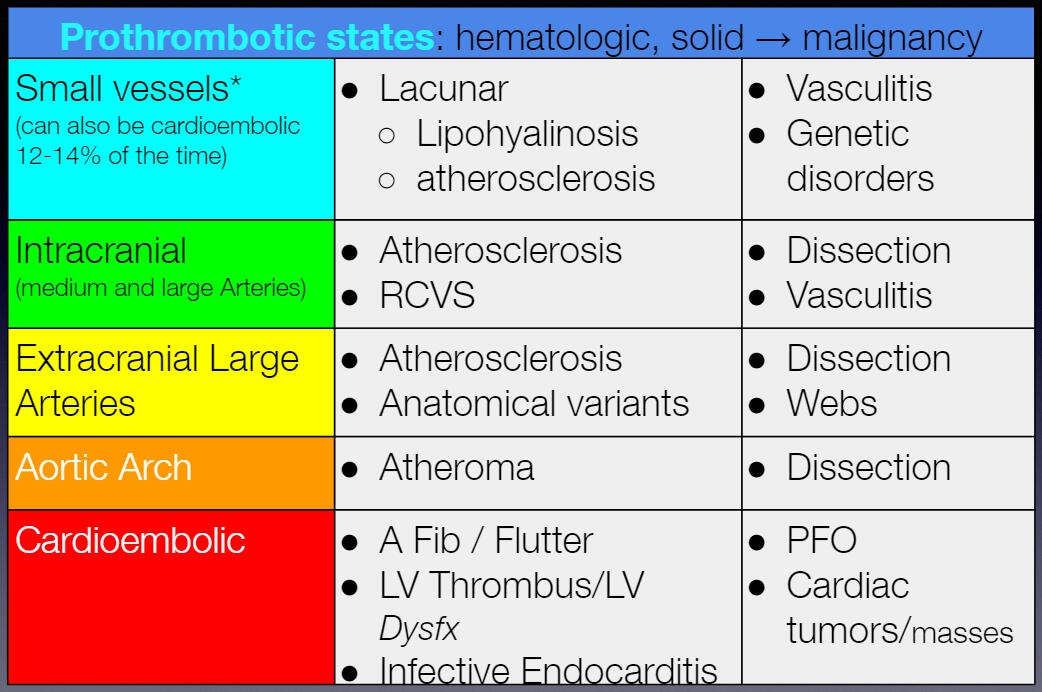
Pathophysiology and Epidemiology
Cardioembolic - secondary to atrial fibrillation
Large vessel atherosclerosis
Small vessel/lacunar strokes - secondary to HTN
Other (more common in young patients <50) - PFO, carotid/vertebral dissections
Cryptogenic/unknown
Source: Dr. Houman Khosravani
Risk factors
HTN
Dyslipidemia
Diabetes
Smoking
Atrial fibrillation
Cardiac disease/PVD
Obesity/reduced physical activity
EtOH misuse
Pro-thrombotic/hypercoagulable state - OCP/hormone replacement use, SLE, APLA, Factor V Leiden, protein C and/or S deficiency, anti-thrombin III deficiency, malignancy
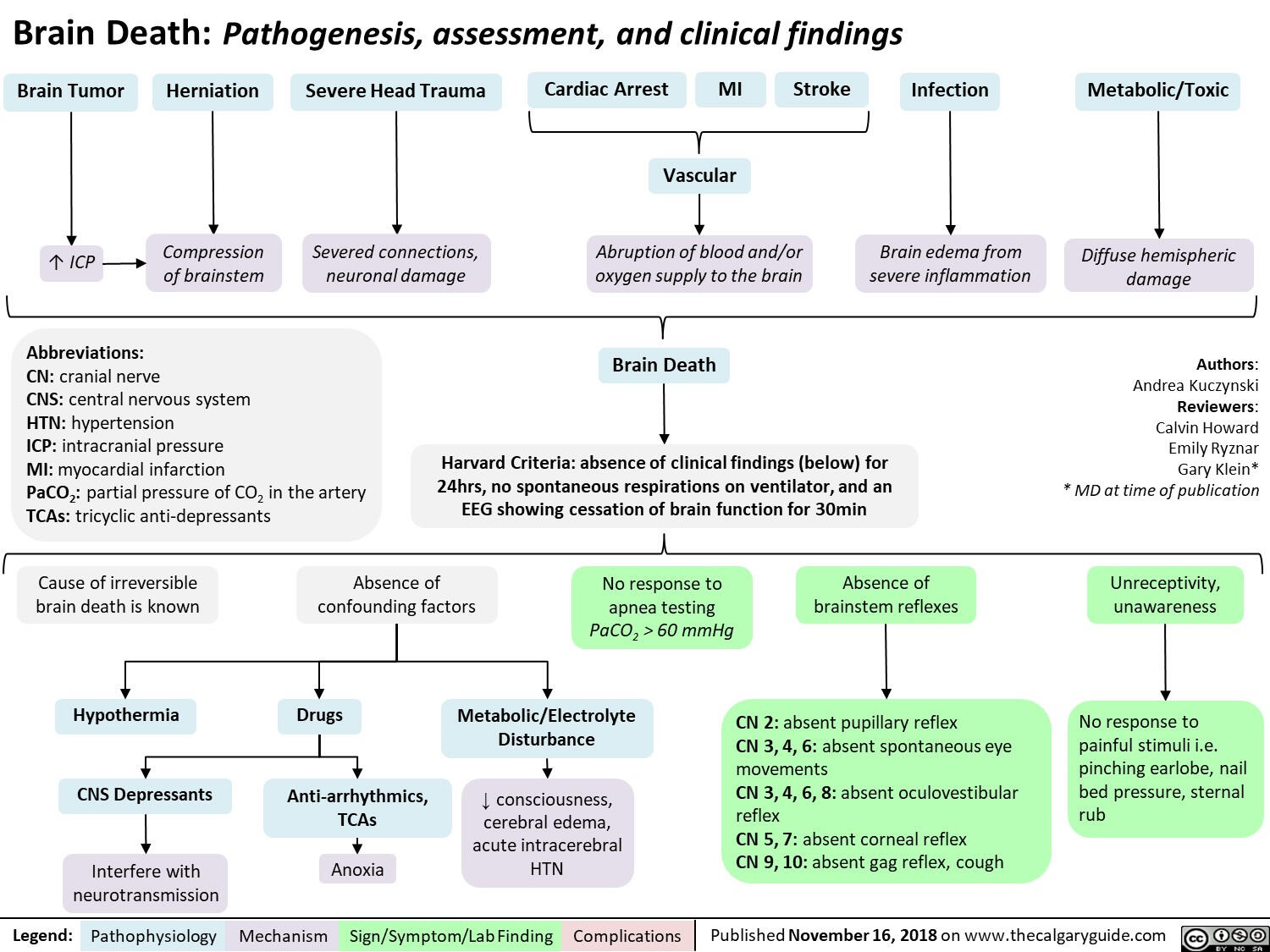
Click image to enlarge
Source: The Calgary Guide to Understanding Disease
⊙ CLINICAL PEARL
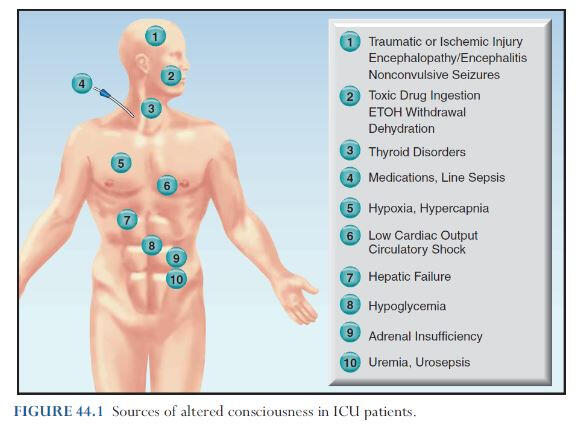
Patients may present with a variety of symptoms including headache, altered mentation, seizure, unilateral and/or brainstem deficits
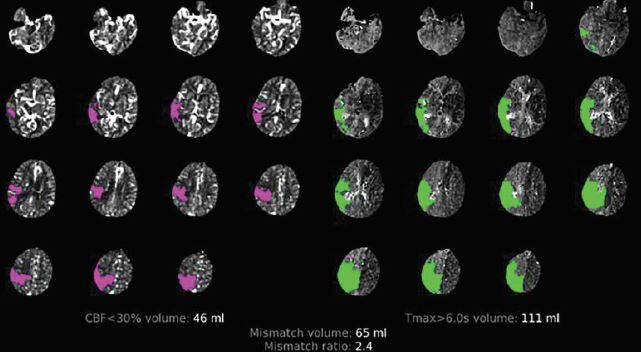
Investigations
Stat CT/CTA/CTP - assess for ischemic changes, hemorrhage, arterial occlusion, perfusion mismatch
NIHSS clinical examination
Vital signs including heart rate and BP
ECG
CBC
Lytes, extended lytes (Mg, Ca, PO4), creatinine
Blood glucose
24 hours after tPA and/or EVT: CT head
MRI brain when clinically stable
Lipid profile
HbA1c
Transthoracic +/- transesophageal echo with bubble study/definity contrast to look for vegetations, intracardiac thrombus, and/or PFO; TEE is for valves/PFO
In appropriate situations, consider cardiac CT for LAA clot
Blood and urine cultures - especially if patient is febrile and has risk factors for endocarditis (i.e., younger age, IVDU
Holter monitor
CT early signs of ischemic stroke:
Hyperdense vessel
Loss of grey-white differentiation
Sulcal effacement
Loss of insular ribbon
Hypoattenuation of deep grey matter nuclei - highly specific for ischemia within 6hrs
Swelling/mass effect
For the ASPECTS score figure see ASPECTS (Alberta Stroke Program Early CT Score) Assessment of the Perfusion–Diffusion Mismatch
CT perfusion:
Assess the core and the penumbra (brain at risk)
Core features: increased MTT, markedly decreased CBF and CBV
Penumbra features: increased MTT, moderately reduced CBF, normal/increased CBV
More likely to have favourable outcome with mismatch ratio >/= 1.8, volume >/= 15mL
Click image to enlarge
[Source: Dr. Phavalan Rajendram Emergency Lecture 2020]
Treatment
Assess patient for stability and call for help from the emergency department/ICU as needed
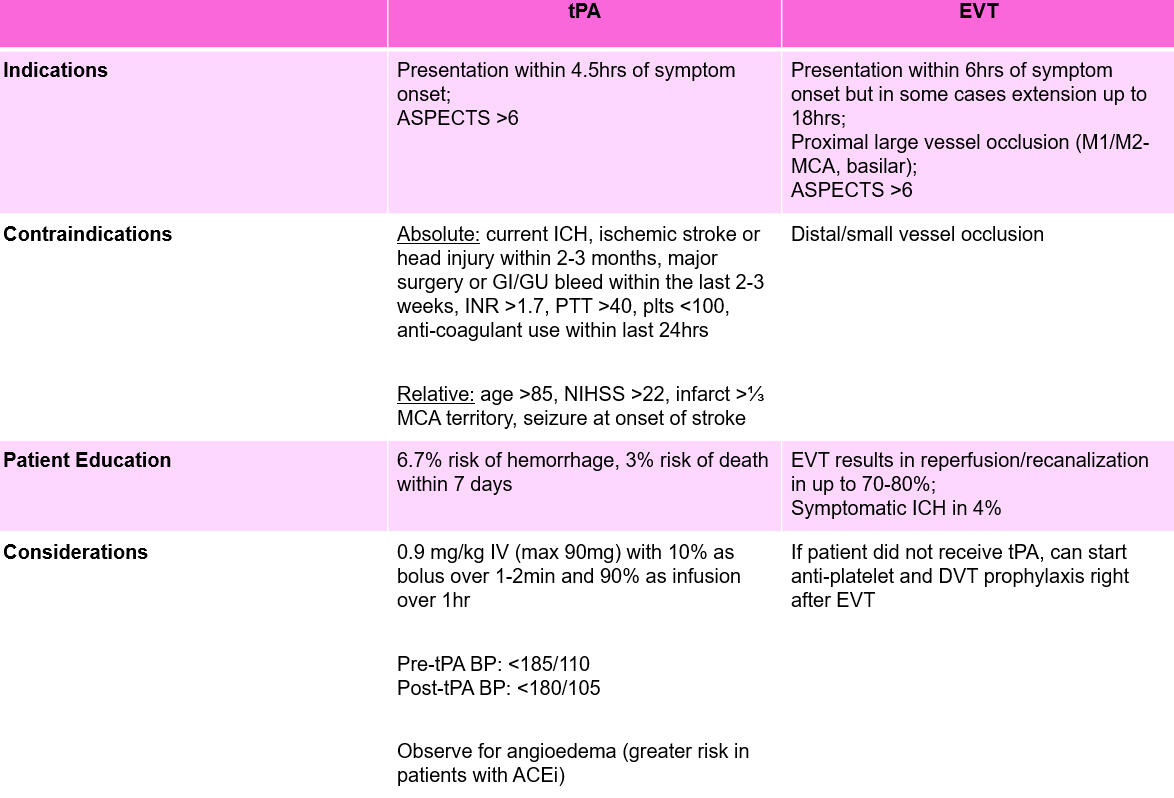
Thrombolysis (TPA/TNK) and/or EVT (see below)
Thrombolysis-angioedema: Solumedrol 125mg IV or Hydrocortisone 200mg IV + Famotidine 20mg IV IV or Diphenhydramine 50mg IV
If clinically stable with stable CT head 24hrs post-intervention (tPA, EVT), can start single anti-platelet and DVT prophylaxis
If NIHSS </= 3 can start dual anti-platelets for 21 days, then monotherapy life-long thereafter (CHANCE, POINT trials)
Starting anti-coagulation post-ischemic stroke (i.e., for AFib): initiation on day 3 (small stroke), 6-7 (medium), or 12-14 (large stroke) but depends on staff and presence of any hemorrhage Reference: Secondary Stroke Prevention Guidelines 7.2
BP: target <140/90 or <130/80 (diabetic patients/small vessel disease)
Dyslipidemia: target LDL <1.8 for those with small vessel disease
Carotid endarterectomy versus stenting in patients with symptomatic large vessel atherosclerosis
Diabetes: target HbA1c <7% (some leniency in patients >80 based on Canadian Diabetes Association)
Must address driving based on residual function as an inpatient!
Lifestyle: cessation of smoking, physical activity, reduced salt intake/DASH diet/Mediterranean diet, reduced EtOH intake
Hemorrhagic Stroke
By Dr. Andrea Kuczynski
Reviewed by Dr. Keithan Sivakumar
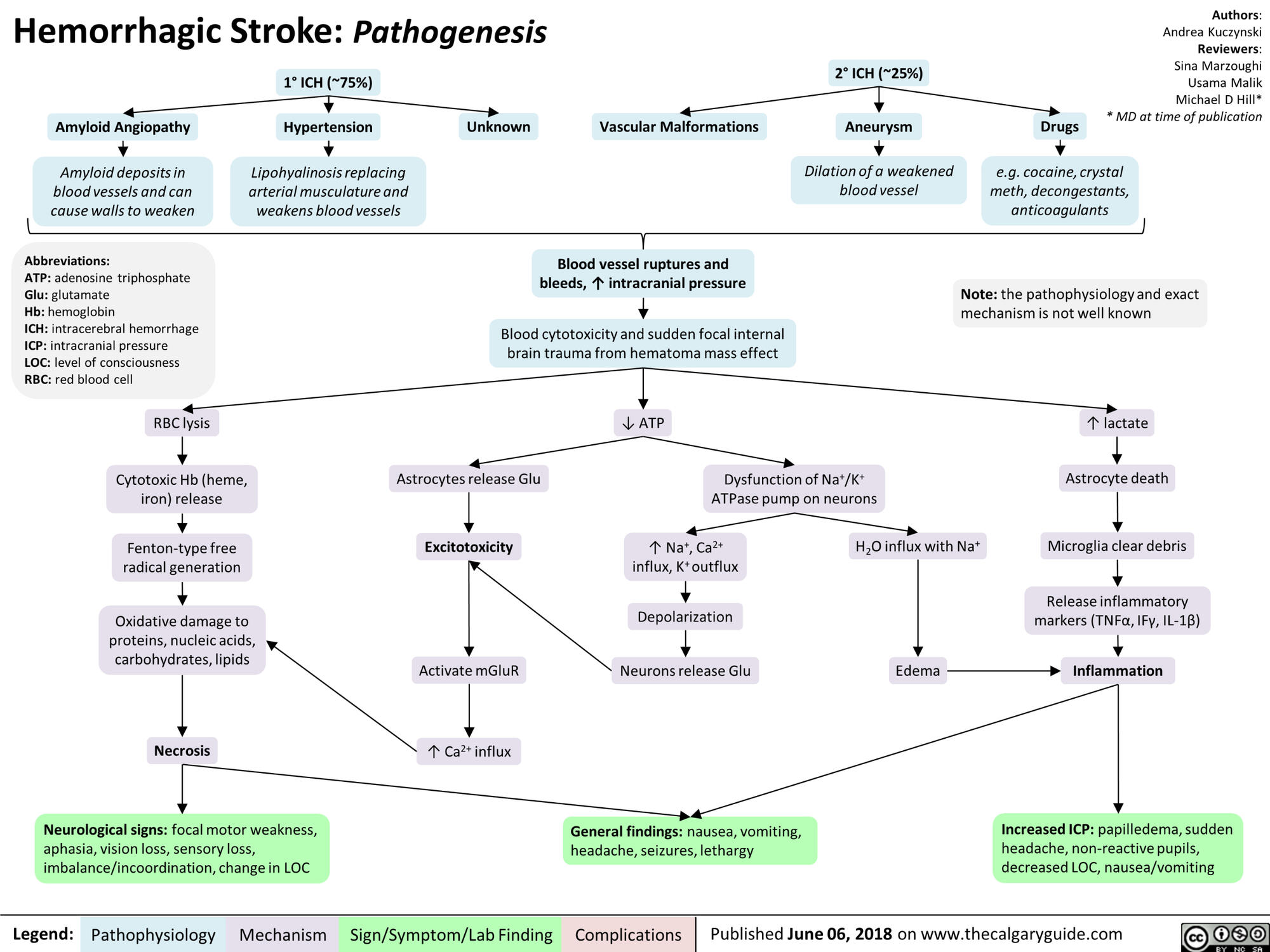
Pathophysiology and Epidemiology
Etiology characterized based on location - lobar (CAA, ischemic stroke with hemorrhagic transformation), deep (HTN, tumor/metastasis), intraventricular (extension from HTN hemorrhage in basal ganglia, aneurysmal rupture, intraventricular AVM/tumor)
Less common stroke type (10-15%) - more common in individuals with hypertension and older adults (presence of CAA)
Risk factors
HTN
Age - > 65
Trauma & Head Injuries
Vascular anomalies - arterial dissection, CVST, AVM, aneurysmal rupture
Tumors/metastasis
Sympathomimetic drugs (e.g. cocaine, amphetamines)
Smoking
EtOH misuse
Family history
Click image to enlarge
Source: The Calgary Guide to Understanding Disease
Clinical Features
Headache - often described as sudden onset & worst headache (thunderclap)
Altered level of consciousness
Nausea/vomiting
Dizziness/vertigo
Focal neurological deficits
Seizure
Investigations
Stat CT/CTA/CTP - assess for ischemic changes, hemorrhage, arterial occlusion, perfusion mismatch
NIHSS clinical examination
ICH score
Vital signs including heart rate and BP
ECG
CBC
Lytes, extended lytes (Mg, Ca, PO4), creatinine
Blood glucose
Blood and urine cultures - especially if patient is febrile and has risk factors for endocarditis (i.e., younger age, IVDU) and subsequent mycotic aneurysms/emboli with hemorrhagic transformation
CT head 6-24 hours after initial presentation
MRI brain when clinically stable with SWI/GRE sequence
Common CT findings in hemorrhage:
Ventricular effacement
Midline shift
Hyperdense blood with surrounding hypodensity (edema)
Spot sign - active bleeding
Treatment
Acute treatment for all ICHs
Acute BP control: SBP <140 (if spot sign present indicating active bleeding) versus SBP <160 (if initial SBP >220 and/or renal dysfunction, absence of active bleeding)
Eventually target BP <140/90 or <130/80 (diabetics)
If patient uses Warfarin, can give Octaplex 1000IU (for patients 50-90kg with INR 1.5-4) and vitamin K 10mg IV push, TXA 1g IV push
Consult Neurosurgery - consideration of EVD and/or decompressive hemicraniectomy if indicated
Avoid secondary brain injury: treat Hb <70, avoid fever, correct coagulopathy
Patients do not require anti-platelets!
Risk factors for poor prognosis: ICH score - older age, initial GCS 3-4, intraventricular hemorrhage, hemorrhage volume >30mL
Stroke in the Young
By Dr. Andrea Kuczynski
Pathophysiology and Epidemiology
Typically considered a “stroke in the young” in an individual <50 years old
Systemic disease associated with prothrombotic state and infarct/hemorrhage: SLE, APLA, vasculitis, Behcet’s, Susac syndrome
| Carotid Dissection | Vertebral Dissection | CVST | Endocarditis | |
|---|---|---|---|---|
| Risk Factors | Head/neck trauma, connective tissue disease (Marfan’s, Ehlers Danlos, fibromuscular dysplasia), neck manipulation (yoga, chiropractor) | Head/neck trauma, connective tissue disease (Marfan’s, Ehlers Danlos, fibromuscular dysplasia), neck manipulation (yoga, chiropractor) | Prothrombotic conditions, hematological disorders, systemic disease (SLE, IBD), incidental finding in trauma cases | Immunocompromised host, IVDU, mechanical/prosthetic valve, atrial myxoma, intracardiac thrombus, marantic endocarditis |
| Clinical Features | Headache, ipsilateral neck pain, possible ipsilateral Horner’s (rare), retinal/cerebral ischemia, pulsatile tinnitus | Headache, nausea/vomiting, vertigo/dizziness, unilateral pain/weakness | Diffuse, acute onset (thunderclap) headache, diplopia secondary to CN6 palsy, nausea/vomiting, altered level of consciousness | Depends on area of infarction; systemic signs including Osler’s nodes, splinter hemorrhages, etc. |
| Investigations | CTA: crescent sign | CTA: crescent sign, double lumen sign | CT/CTV: delta sign/empty delta sign, subarachnoid hemorrhage, dense cord sign | CT/CTA: may see mycotic aneurysms |
| Treatment | Single anti-platelet (CADISS trial) | Single anti-platelet (CADISS trial) | Anti-coagulation | Treat underlying endocarditis |
Clinical Features
See ischemic stroke and hemorrhagic stroke for full description of focal neurological deficits
Investigations
See ischemic stroke section for basic blood work, neuroimaging, and standard stroke investigations
Autoimmune work-up: ESR/CRP, ANA, anti-dsDNA, ENA, RF, C3/C4, cryoglobulins
Pro-thrombotic/hypercoagulable state work-up: APLA (anti-cardiolipin, B2-glycoprotein-1, lupus anticoagulant), Factor V Leiden, protein C and/or S deficiency, anti-thrombin III deficiency, testicular U/S in males, CT chest/abdo/pelvis for malignancy work-up
Infectious work-up: VDRL, HIV serology
Treatment
Depends on etiology (see table above for examples)
Cognitive Neurology
Normal Pressure Hydrocephalus (NPH)
By Dr. Calvin Santiago
Pathophysiology and Epidemiology
Caused by build-up of CSF
Idiopathic NPH (iNPH): Unknown etiology
Secondary NPH (sNPH): Due to conditions impairing CSF absorption (e.g. SAH, brain tumors)
Clinical Features
Insidious onset of changes starting with gait, then urinary and/or cognitive changes
Initially develops non-specific gait difficulties (slowing of gait, feeling imbalanced) before developing difficulties with initiating of gait (previously known as magnetic gait) or increased falls due to postural instability
May start with increased urinary frequency, than urgency, and finally incontinence
Cognitive impairment includes difficulties in executive dysfunction (e.g. multitasking, judgement)
Neuro-imaging Features
Ventriculomegaly present
DESH (disproprotionately enlarged subarachnoid hydrocephalus)
Crowding present
Transependymal flow present
Significant ischemic white matter changes present
Evans index >0.3
Callosal angle between 40º and 90º
Questions to consider
Are there secondary causes of NPH? (e.g. Head trauma, meningitis, SAH, ICH, tumors)
Does the patient have arthritis, spinal disease, pain/sensory symptoms, or other causes (e.g. poor vision, hearing, parkinsonism) that also explains gait difficulties?
Are there other confounders to diagnosis? (e.g. Sleep apnea, fecal incontinence, headaches, REM sleep disorders, orthostatic hypotension, anosmia)
Was gait difficulty before or after cognitive decline? - Gait onset before or at same time as cognitive changes has a good prognosis of shunting, not true if cognitive decline occurred prior to gait changes
How long have they had cognitive changes and do they have other comorbid cognitive dysfunction? - 2+ years of cognitive decline indicates poor prognosis with shunting
Investigations
UHN NPH protocol developed by Dr. Tang-Wai and Dr. Fasano - for use at UHN but can be used as a reference guide at other sites (i.e. but should not be printed and placed in patient's chart)
Physical exam to assess for orthostatic hypotension, extraocular eye movements, parkinsonism, UMN presence, and peripheral neuropathy
MRI Brain with sagittal FIESTA sequence
Need high clinical suspicion of NPH before proceeding with the NPH assessment
NPH assessment
Pre and post- MOCA with semantic fluency (e.g. animals), and naming (BNT-15)
Pre- video recording of gait (stand up from chair, walk towards camera for at least 10 meters, turn, walk back to chair, repeat)
Large volume lumbar puncture (30-40 cc)
1 hour post-LP - Video record of walk
3 hour post-LP - Video record of walk
** Note: Gait is best performed at a Gait Lab to determine if gait is improved/changed
Treatment
If patient demonstrates improvement of gait post large-volume LP, they should be referred and assessed by Neurosurgery for possible shunt
Patient Education
Unfortunately, prognosis can still be poor without guarantee for improvement post-surgery and there can significant complications including infections and shunt malfunctions post-operatively
VP shunt’s main purpose is improvement in gait and urinary incontinence but NOT cognitive impairment
CREUTZFELD-JAKOB DISEASE
By Dr. Andrea Kuczynski
Pathophysiology and Epidemiology
Rapidly progressive dementia due to prion disease (conformational change of proteins)
Sporadic CJD: age 55-70 years, mean 64 years
Variant CJD: mean 26 years, longer duration of symptoms >6 months
Iatrogenic CJD: rare, due to dura mater transplantation
Heidenhain variant CJD: targeting of prions to occipital lobe
Fatal Familial Insomnia: 50's, progressive sleep and autonomic disturbances (hypertension, tachycardia, hyperhidrosis), ataxia
Gerstmann-Straussler-Scheniker: 40-50's, progressive cerebellar ataxia, dysarthria, nystagmus and then with cognitive and UMN symptoms
Clinical Features
Altered level of consciousness/mental status
Psychosis - delusions, hallucinations
Progressive cognitive impairment
Myoclonus
Seizures
Cortical visual disturbances (especially in Heidenhain variant CJD) - disturbed perception of colours or structures, optical distortions, hallucinations
Cerebellar ataxia
Extrapyramidal symptoms
Investigations
MRI brain - diffusion restriction in striatum and cortex (cortical ribboning), pulvinar sign, Hockey stick sign
LP - RT-QuIC assay with elevated 14-3-3 tau
EEG - periodic sharp wave complexes and triphasic components
Differential of cortical ribboning/striatal involvement:
Acute severe hepatic encephalopathy
Autoimmune encephalitis
Hypoglycemic brain injury
Hypoxic ischemic encephalopathy
Mitochondrial disease
Post-ictal state
Extrapontine osmotic demyelination
EBV encephalitis
Treatment
Supportive care
Management of comorbidities and symptoms (i.e., anti-epileptic medication)
Patient and family counseling
Patient Education
Average survival 6-7 months from diagnosis for most cases of CJD, although GSS can be longer (years)
Early involvement of the thalamus is a poor prognostic sign
Neuromuscular & Peripheral Neuropathies
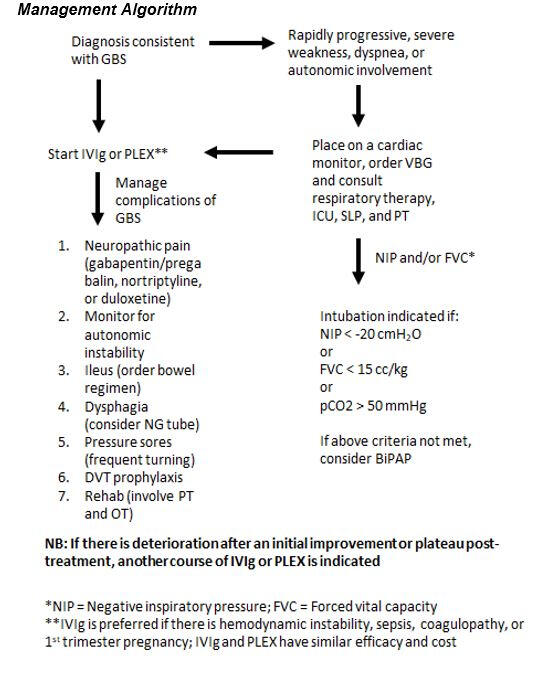
Guillain-Barre Syndrome (GBS)
By Dr. Elliot Cohen
Reviewed by Dr. David Fam
Pathophysiology and Epidemiology
AIDP - Acute or subacute onset autoimmune demyelinating polyradiculoneuropathy - often thought to be preceded by respiratory or GI infection
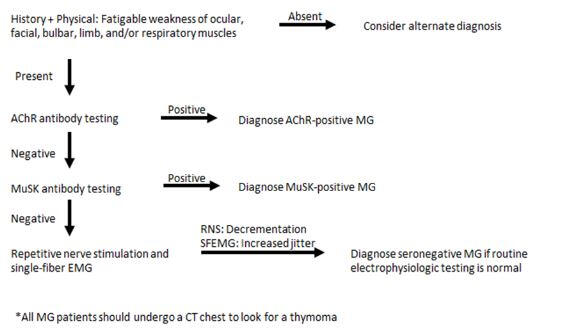
Clinical Features
Numbness/paresthesias and weakness beginning in the legs, progressing proximally, commonly involving the face, eyes, and respiratory muscles (sensory symptoms are less pronounced than weakness)
Onset is over the course of days with rapid progression to possible quadriplegia in a few days, with maximum weakness achieved in 2-4 weeks
Hyporeflexia or areflexia
Neuropathic pain in lower back and thighs
Autonomic involvement, such as tachy/bradycardia, hyper/hypotension, gastric hypomotility, and urinary retention
70% of cases are preceded by respiratory or gastrointestinal infection. Less common precipitants are pregnancy, vaccination (controversial), surgery, or cancer
⊙ CLINICAL PEARL
Often the reflexes in GBS are absent in the setting of initially mild or moderate weakness - if someone is already paralyzed, reduced reflexes may not offer much information since some strength in a muscle is necessary for a reflex. However, if someone has 4/4+ strength but absent reflexes, this suggests a demyelinating process
GBS Variants
Acute motor axonal neuropathy (AMAN)
Acute motor-sensory axonal neuropathy (AMSAN)
Miller-Fisher syndrome (Triad of ophthalmoparesis, ataxia, and hyporeflexia)
Paraplegic variant
Pharyngeal-cervical-brachial variant
Red flags for other causes (not GBS)
HIV
Rash
Severe pain
Pupillary involvement
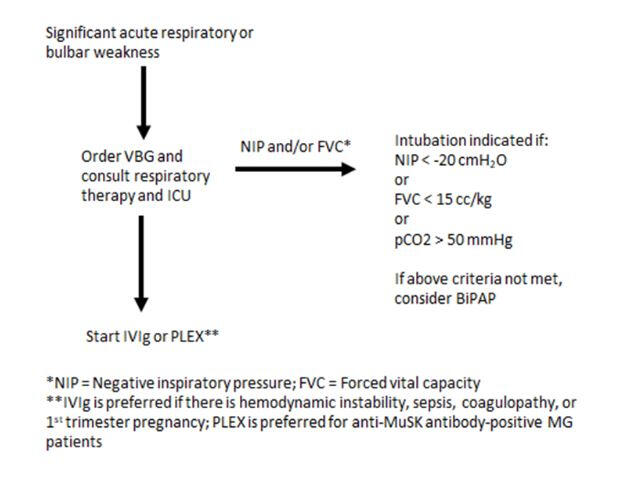
Investigations
If concern for severe weakness, dyspnea, autonomic involvement - telemetry, VBG, consult RT, SLP, PT +/- ICU
ANA
SPEP with immunofixation and free light chains
HBA1c
ESR/CRP
Lumbar puncture (Cell count, Protein & Glucose, Cultures, Cytology & Flow Cytometry) - CSF analysis may show albuminocytologic dissociation (increased total protein without an increase in WBC)
MRI Spine with GAD (may see nerve root enhancement)
EMG/NCS (may show prolonged/absent F waves, temporal dispersion prolonged distal latencies, sural nerve sparing)
Consider: Lyme, HIV, CMV, ACE for other infectious/inflammatory causes
Treatment
Acute therapies
Usually IVIG is started instead of PLEX first
Intravenous Immunoglubulin (IVIg)
For severe exacerbation or prior to surgery if preo-operative bulbar/respiratory symptoms (Onset 3- 10 days, benefits weeks to months)
Dosing: 2g/kg IV over 2-5 days
Side effects: Infusion reactions, allergic reaction, aseptic meningitis, thromboembolic events, hemolytic transfusion reactions
Plasma Exchange (PLEX)
For severe exacerbation or prior to surgery if preo-operative bulbar/respiratory symptoms (Onset 1 - 5 days, benefits 1 - 3 months)
Dosing: 4-6 exchanges
Side effects: Hypocalcemia, hypotension, febrile/allergy, immunosuppression (if septic, give IVIg instead if indicated)
AVOID PLEX AFTER IVIg - otherwise you will be removing IVIg from patient’s system
Click image to enlarge
CIDP
By Dr. Caz Zhu
Pathophysiology and Epidemiology
Chronic inflammatory demyelinating polyradiculoneuropathy - similar to AIDP (e.g. GBS) except duration of symptoms can be over months or relapsing-remitting
Can initially present as GBS with severe weakness but progression is longer ( > 4 weeks)
Can be associated with HIV, paraprotein, inflammatory disease, malignancies
Clinical Features
Similar symptoms to that of AIDP/GBS with ascending sensory and motor symptoms (proximal and distal weakness) as well as areflexia Symptom progression beyond the 4 weeks seen in GBS (thus; important to change differential if GBS is persistent and worsening > 1 month)
Often have other features such as tremors, cranial nerve/bulbar findings, increased ICP
The differential for diseases like CIDP can also include the following:
| Diseases | Clinical features | Investigations |
|---|---|---|
| POEMS (Polyneuropathy, organomegaly, endocrinopathy, monoclonal plasma cell disorder, skin changes) | - Diffuse peripheral neuropathy; distal sensory symptoms with proximal & distal weakness with organomegaly, osteosclerotic bone lesions, castleman's disease, endocrine abnormalities (hypothyroid, diabetes), and skin changes (hyperpigmentation, telangiectasia, raynaud's) | - SPEP and immunofixation, Skeletal survey, VEGF levels |
| CISP (Chronic immune sensory polyradiculopathy) | - Prominent sensory ataxia | - Similar to CIDP |
| MMN (Multifocal motor neuropathy) | - PURE MOTOR - Asymmetric with multiple neuropathies; with cramps, and fasciculations WITHOUT UMN findings | - Anti-GM1 antibodies |
| MADSAM (Multifocal acquired demyelinating sensory and motor neuropathy) | - Insidious, asymmetrical, upper extremity symptoms & cranial nerve involvement (CN 2,3,5,7) | |
| DADS (Distal acquired demyelinating and symmetrical neuropathy) | - Slowly progressive and indolent with sensory predominance; symmetrical distal > proximal symptoms favoring lower extremities; often with ataxia and tremors | - anti-MAG antibodies |
Investigations
If concern for severe weakness, dyspnea, autonomic involvement - telemetry, VBG, consult RT, SLP, PT +/- ICU
ANA
SPEP with immunofixation and free light chains *
HBA1c
ESR/CRP
Lumbar puncture (Cell count, Protein & Glucose, Cultures, Cytology & Flow Cytometry) - CSF analysis may show albuminocytologic dissociation (increased total protein without an increase in WBC)
MRI Spine with GAD (may see nerve root enhancement)
EMG/NCS (may show prolonged/absent F waves, temporal dispersion prolonged distal latencies, sural nerve sparing)
Consider: Lyme, HIV, CMV, ACE if concern for another process
CIDP panel - download requisition - Contactin-1, Neurofascin-155, CASPR1
** If + for IgG or IGA lambda monoclonal gammopathy - consider skeletal survey and VEGF for possible POEMs*
Treatment
First line treatment include IVIG and PLEX (see GBS section)
Corticosteroids also considered depending on response to IVIG/PLEX - can consider steroid pulse x 5-7 days and then start prednisone 1mg/kg for 1-2 months before tapering
"Treatment resistant" - can consider cyclophosphamide but patients with antibodies to contactin-1 and neurofascin can benefit better from PLEX/B-cell depleting therapies (Rituximab)
POEMS - treatment is with targeted radiation (limited disease) or chemotherapy/stem cell transplant
Myasthenia Gravis
By Dr. Elliot Cohen
Reviewed by Dr. David Fam
Pathophysiology and Epidemiology
Autoimmune disease affecting post-synaptic proteins at neuromuscular junction - impairs binding of acetylcholine to receptor
Common Myasthenia Gravis antibodies include: Anti-ACHr (80-85%) and MuSK (8%)
More often seen in younger females and older males
Patients with MG may also have a thyoma
Clinical Features
Classic presentation is fatigable weakness of muscles - patients may endorse that symptoms worsen with activity (e.g. diplopia worse with reading, dysarthria if they talk for a long period of time)
Most common presenting symptoms:
| Weakness | Clinical presentation |
|---|---|
| Ocular weakness - most common | Diplopia, ptosis (may be asymmetric) |
| Facial weakness | Eye closure weakness, “sad” facial appearance |
| Bulbar weakness | Dysarthria (nasal speech), dysphonia, dysphagia, difficulty chewing over time |
| Limb Weakness | Loss of strength in different muscle groups (arms, legs, neck) |
| Respiratory weakness | Orthopnea |
Patients may have ocular myasthenia gravis but this can “generalize” to affect elsewhere
Myasthenia Gravis can be exacerbated by: stress, illnesses, fever, hypothyroidism/hyperthyroidism, menstruation, drugs
Myasthenic Crisis
Life-threatening exacerbation of MG with worsening muscle weakness leading to respiratory failure
Clinical signs of an impending crisis include - prominent bulbar involvement, neck and deltoids weakness, changes in respiration
Need urgent evaluation and measurement of respiratory parameters (FVCs)
Indications for intubation include: FVC < 15 ml/Kg, PEmax < 20 cmH2O, Pmax less than -20 cmH2)
Physical Exam
Ptosis
Frontalis activation to compensate for ptosis
If asymmetric ptosis, lifting the obviously ptotic eyelid may bring out ptosis on the other side as the frontalis activation relaxes
Sustained upgaze for 1 minute with worsening of ptosis (diplopia will worsen at 15-30 seconds)
Ice-pack test: Hold ice against ptotic eye for 2-5 minutes. Improvement of ptosis is expected
Facial and neck weakness
Inability to bury the eyelashes upon eye closure with subsequent “peek sign” (sclera becomes visible as eye closure weakens)
Ability of examiner to open jaw against resistance (jaw closure is weaker than jaw opening)
Testing power for neck flexion and extension
Diplopia
Binocular diplopia with any combination of extraocular movement abnormalities (though downgaze typically spared)
Single breath count
Count to 20 at 2 Hz on one breath. If able to do so, respiratory weakness is unlikely. Also listen for nasal dysarthria
Limb power
Repeatedly test power in deltoids, triceps, or hip flexors, assessing for fatigability
Investigations
CBC, LFTs, HbA1c
Repetitive nerve stimulation and single-fiber EMG
CXR → CT Chest to rule out thyoma
AChR and MuSK antibody testing (Mitogen requisition forms or BC Neuro requisition forms)
If concern for respiratory weakness - VBG and consult RT +/- ICU , FVCS daily - TID (see above for indications for intubation for myasthenic crisis)
Refer for thymectomy if thymoma present (although can consider trhymectomy for non-thymomatous myasthenia gravis - see below in treatment)
Click image to enlarge
Treatment
Symptomatic management
Pyridostigmine (Mestinon): Acetylcholinesterase inhibitor
Temporary symptomatic improvement of symptoms (onset of action: 20-30 minutes)
Starting dose: 30 mg PO q4-6 hours (can increase by 30-60 mg every 1-2 weeks up to a maximum of 480 mg/day)
Side effects: Nausea, vomiting, diarrhea, secretions
May worsen symptoms in patients with anti-MuSK antibody-positive MG
Can increase secretions in patients in MG crisis - often held in the ICU setting
Myasthenic Crisis
Intravenous Immunoglubulin (IVIg)
For severe exacerbation or MG crisis (onset of action: 3-10 days, benefits last weeks to months)
Dosing: 2g/kg IV over 2-5 days
Side effects: Infusion reactions, allergic reaction, aseptic meningitis, thromboembolic events, hemolytic transfusion reactions
Plasma Exchange (PLEX)
For severe exacerbation or MG crisis (preferred to IVIg in anti-MuSK antibody-positive MG) (onset of action: 1-5 days, benefits last 1-3 months)
Dosing: 4-6 exchanges
Side effects: Hypocalcemia, hypotension, febrile/allergy, immunosuppression
AVOID PLEX AFTER IVIg - otherwise you will be removing IVIg from patient’s system
Click image to enlarge
Disease-modifying therapy
Prednisone
First line disease modifying therapy for intolerable symptoms or risk of deterioating respiratory/bulbar function
Starting dose for ocular - mild generalized MG: 10-20 mg PO daily
Starting dose for moderate-severe generalized MG: 0.5 - 0.75 mg/kg/day (start at 10 mg PO and increase by 10 mg every 3-5 days)
Starting dose for intubated patients: 100 mg PO daily
There can be a phenomenon of transient prednisone associated weakness that patients experience when first starting prednisone
Adverse effects: Sleep disturbance, mood changes, weight gain, GI irritation, avascular necrosis
Patient should also be on Vitamin D and Calcium
Patients may require PJP prophylaxis and should have TB, hepatitis B, and strongyloides testing prior to initiation of prednisone
Other disease modifying therapies (steroid-sparing) include:
Azathioprine
Mycophenolate mofetil
Cyclosporine
Tacrolimus
Rituximab
NEW TREATMENTS - Eculizumab, Ravulizumab, Efgartigimod
Thymectomy
Should be considered in patients who are found to have a thymoma and ACHr +
Can also be considered in patients < 55 who have moderate-severe generalized MG for < 2 years who may not be adequately controlled with symptomatic management
Patient Education
Counsel patients on medications to avoid that can exacerbate MG
Drugs that exacerbate MG
Absolutely contraindicated - Alpha-interferon, botulinum toxin, D-penicillamine, telithromycin
Relatively contraindicated:
| Drug class | Specific drugs |
|---|---|
| Antibiotics | Macrolides, fluoroquinolones, aminoglycosides |
| Antiepileptics | Phenytoin, gabapentin, barbiturates |
| Beta-blockers | Including eye drops |
| Calcium-channel blockers | - |
| Magnesium salts | MgSO4 , MgOH |
| Lithium | - |
| Anti-arrhythmics | Procainamide, quinidine |
| Anti-malarials | Quinine, hydroxychloroquine |
| Paralytics | Succinylcholine, rocuronium |
| Statins | Atorvastatin, Rosuvastatin - Can use at lowest possible dose with monitoring |
| Respiratory depressants | Benzos, Opiates - Monitor for respiratory depression |
Lambert-Eaton Myasthenic Syndrome (LEMS)
By Dr. Elliot Cohen
Reviewed by Dr. David Fam
Pathophysiology and Epidemiology
Autoimmune disease affecting pre-synaptic voltage gated calcium channels (VGCC) - impairs release of acetylcholine into synaptic cleft
Can be either primary autoimmune or paraneoplastic (almost always associated with small cell lung cancer in adults)
Common antibodies: anti-VGCC found in 90% of patients
Age of onset - bimodal peak at ~35 and 60
Clinical Features
Prominent proximal weakness that progresses distally
Areflexia (but reflexes improve with sustained voluntary contraction)
Autonomic dysfunction: Dry mouth & eyes, constipation, erectile dysfunction, orthostatic hypotension, pupillary abnormalities
Investigations
anti-VGCC antibody testing (Mitogen requisition forms)
NCS and EMG
CT Chest to assess for SCLC
Refer to oncology for management of underlying SCLC if paraneoplastic
Treatment
Symptomatic management
3,4-Diaminopyridine (3,4 DAP)
Increases pre-synaptic release of Ach by blocking K+ channel, onset of action 30-90 minutes
If patient improves, no need for another treatment
Starting dose: 5-10 mg PO TID or QID (can increase to max 100 mg/day)
Side effects: Risk of seizures with > 100 mg/day, paraesthesia, nausea, palpitations
Disease-modifying therapy
Consider IVIG, PLEX, immunotherapy
** For paraneoplastic LEMS - immunosuppression not recommended given risk of tumor progression **
Bell's Palsy
By Dr. Conrad Eng
Reviewed by Dr. David Fam
Pathophysiology and Epidemiology
Thought to be virally mediated by reactivation of HSV1 infection of the facial nerve
Clinical Features
Spontaneous, acute (can occur within hours), isolated unilateral facial palsy - since it’s lower motor neuron pattern of weakness, there should be weakness in BOTH upper and lower part of the face (e.g unlike a stroke where a facial droop is ‘forehead sparing’)
Patients may endorse a slight ear pain behind the ear during the onset
Patients may endorse difficulties closing eye, smiling, difficulty eating, decreased taste
Symptoms occur over 72 hours and gradually recover over months
As symptoms improve, synkinesis can occur due to aberrant regeneration of facial nerve (e.g. eye closing when smiling)
Red flags of atypical Bell’s Palsy
Gradual onset (slowly progressive over weeks and other cranial nerve involvement) - consider neoplastic cause
Vertigo, hearing loss, tinnitus - consider CPA angle mass/lesion
Bilateral facial nerve palsy - consider other infectious causes e.g. Lyme
Vesicles in external auditory canal, tympanic membrane, orophyrynx - Ramsay Hunt
Sensory symptoms - usually Bell's Palsy have more weakness than sensation difficulties
Extraocular eye movement abnormalities
Investigations
Usually a clinical diagnosis but if red flags are present, consider MRI brain +/- GAD
If suspicious for Lyme disease - can send for serological testing
Treatment
Eye care: given poor eyelid closure/tearing from facial palsy - consider artificial tears applied regularly, ointment, patches
Corticosteroids: given within 72 hours of symptom onset - 60-80 mg/day for 1 week
Adverse effects: Sleep disturbance, mood changes, weight gain, GI irritation, avascular necrosis
Patient should also be on Vitamin D and Calcium
Antiretrovirals: no clear evidence to be used with steroids but can consider: valcyclovir 1000 mg TID for 1 week - use with caution in patients with renal failure
Patient Education
Prognosis is good, 85% of patients recover within 3 weeks and if facial function does not return within 3-4 months, consider another diagnosis
Even after the disease is treated, there may still be asymmetry of the face and synkinesis with facial movements
Neuropathy
Can be divided into two categories - focal neuropathy (one nerve/root involvement) vs multifocal neuropathy (subdivided even further into three sections - see below)
Focal neuropathy
Can be focal mononeuropathy (affecting one nerve, e.g. carpal tunnel syndrome) or radiculopathy (affecting one nerve root e.g Disc herniation) or plexopathy (affecting plexus - e.g. Parsonage Turner)
Symptoms include numbness, paraesthesia, pain, and weakness that follows the distribution of the nerve or root
Usually due to a compressive or traumatic etiology
Note:
In Common Upper Extremity Mononeuropathies: Covers carpal tunnel, ulnar and radial neuropathy
In Common Lower Extremity Mononeuropathies: Covers lumbrosacral radiculopathy and foot drop (peroneal neuropathy)
Multifocal neuropathy
Polyneuropathy
Sensory symptoms (paraesthesia then numbness, usually vibration/proprioception affected first) with motor symptoms later in onset, length-dependent pattern (glove and stocking), reflexes diminish in ascending pattern
Often have autonomic dysfunction (e.g. decreased sweating in the feet, orthostatic hypotension, erectile dysfunction)
DDx: Toxic/metabolic causes (Diabetes, EtOH), Genetics (CMT)
Mononeuropathy multiplex
Presentation similar to multiple focal neuropathies
Often has a patchy pattern of sensory and motor symptoms, asymmetrical, nerves affected at different times, and subacute in onset
Unlike polyneuropathy, often have motor symptoms > sensory symptoms, asymmetrical reflexes, and occasionally cranial nerve involvement
DDx: Vasculitis (polyarteritis nodosa, eGPA, Sjogren's), Sarcoidosis
Generalized
** Similar to polyneuropathy but more acute /subacute in onset with possible involvement of cranial nerves
DDx: GBS, CIDP
Common upper extremity mononeuropathies
By Dr. Conrad Eng and Dr. Caz Zhu
Upper extremity anatomy
Nerve roots supplying brachial plexus are C5-T1
| Nerve | Nerve roots | Muscle innervation |
|---|---|---|
| Axillary | C5-C6 | Deltoids |
| Musculocutaneous | C5-C6 | Biceps |
| Median nerve | C6-T1 | Pronator teres, flexor carpi radialis, LOAF (lumbricals 1+2, opponens pollicis, abductor pollicis brevis, flexor digitorum superficialis) |
| Anterior interosseous branch of median nerve | C8-T1 | Flexor pollicis longus, flexor digitorum profundus 1 + 2 |
| Ulnar nerve | C8 - T1 | Flexor carpi ulnaris, flexor digitorum profundus 3+4, adductor pollicis, lumbricals 3+4, dorsal + palmar interossei, opponens digiti minimi, flexor digiti minimi, abductor digiti minimi |
| Radial nerve | C5-C7 | Brachioradialis, triceps, extensor carpi radialis |
| Posterior interosseous branch of radial nerve | C6-C8 | Supinator, extensor carpi ulnaris, extensor digitorum, extensor pollicis longus, extensor pollicis brevis, extensor indicis, extensor digiti minimi |
Carpal Tunnel Syndrome
Pathophysiology and epidemiology
Common entrapment of the median nerve in the carpal tunnel of the wrist
Often affect women more than men
Can be idiopathic but other mechanisms include repetitive stress injury (wrist usage), edema, inflammation, or trauma to the wrist
Risk factors include obesity, pregnancy, aromatase inhibitors, acromegaly, and other medical conditions (e.g. diabetes, arthritis, hypothyroidism, infiltrative disorders, connective tissue disorders)
Clinical Features
Sensory symptoms: Can have pain, numbness, or paraesthesia of the hands (often noted in textbooks that it involves the distal thumb and 2nd + 3rd digits but spares the palmar aspect of the thumb since palmar sensory branch does not pass through carpal tunnel - however, patients may not always state that)
Some patients may endorse tingling radiates up to the shoulder at night when symptoms are severe
Motor symptoms: Difficulties holding objects if severe, thumb abduction weakness - if severe, will appreciate thenar atrophy
Key symptom is whether patients may complain of pain and paraesthesia waking them up at night or in the morning and improved with shaking/wringing of the hands
Provocative maneuvers for CTS: Phalen and Tinel
Physical exam
If suspicious for carpal tunnel syndrome:Motor findings:
Thumb abduction (APB) should be weak (Carpal tunnel - Median)
Thumb flexion (FPL) and pronation of forearm (Pronator Teres) should be normal (Proximal Median)
Elbow flexion (biceps) should be normal (C6)
Elbow extension should be normal (C7)Sensory:
Digits 1-3 of hand that spares the thenar eminence
Positive Phalen's (forcefully flex wrists and hold for 30 seconds)
Positive Tinel's (can be a false positive at times)
Negative Spurling's (radiculopathy pain)Reflexes:
Biceps, triceps, and brachioradialis reflex should be normal
Investigations
EMG/NCS
Treatment
Individualize treatment based on how severe nerve compression is as determined by electrodiagnostic findings
If mild-moderate - consider wrist splints at night and NSAID treatment for pain
If severe with significant motor deficits - carpal tunnel release surgery for those of whom nonsurgical therapies have failed
Ulnar neuropathy
Pathophysiology
Entrapment of the ulnar nerve at the elbow is second most common compressive neuropathy (compression at wrist (Guyon’s canal) is less common)
Usually due to compression or stretch at the groove of the elbow or cubital tunnel
Other etiologies include trauma and masses at the site (e.g. tumors, ganglias)
Clinical Features
Motor symptoms: Weak grip, dexterity, pinch strength and there may be atrophy of hypothenar and thenar (but thumb abduction will be spared)
Sensory symptoms: Pain, numbness and paraesthesia along the pinky and 4th digit of fingers
Provocative maneuvers: Tinel’s test on elbow
Physical exam
If suspicious for ulnar neuropathy:Motor findings:
Pinky flexion weakness (FDM), Finger abduction/adduction weakness (Dorsal/palmar interossei), and thumb adduction weakness (adductor pollicis) (Ulnar nerve)
Thumb abduction (APB) should be normal (Median nerve)
Thumb flexion (FPL) should be normal (Anterior Interosseous Nerve/C8)
Extension of index (EIP) should be normal (Radial nerve)Sensory:
Digits 4+5 and ulnar border of hand affected
Positive Phalen's (forcefully flex wrists and hold for 30 seconds)
Positive Tinel's (can be a false positive at times)
Hand postures
1. Benediction posture: Clawing of ring and little finger (due to weakness of third and fourth lumbricals) and fingers and thumbs abducted (adductor pollicis weakness)
2. Wartenberg’s sign: Abducted little finger (weakness of interosseous muscle)
3. Froment’s sign: Difficulty pinching a piece of paper
Investigations
EMG/NCS
Treatment
Individualize treatment based on how severe nerve compression is as determined by electrodiagnostic findings
If mild-moderate - consider wrist splints at night and NSAID treatment for pain, avoid leaning on elbow
If severe with significant motor deficits - could consider surgery for cubital tunnel release
Radial neuropathy
Pathophysiology
Radial neuropathies are divided into three lesions: at the axilla, spiral groove, or below the elbow (posterior interosseous neuropathy)
Most common neuropathy is a lesion at the spiral groove due to compression or prolonged immobilization (e.g. Saturday night palsy)
Radial neuropathies at the axilla are due to prolonged compression (e.g. crutches)
Posterior interosseous neuropathy (PIN) may be due to entrapment
Clinical Features
Wrist drop is often the presenting chief concern
Radial neuropathy at spiral groove: wrist drop and finger drop, weakness in supination, sensory loss in lateral dorsum of hand and fingers
Radial neuropathy at the axilla: Motor weakness as above WITH arm extension weakness and sensory loss extending to posterior forearm and arm
Posterior interosseous neuropathy demonstrates reduction in wrist extension with radial deviation and NO SENSORY LOSS
If symptom onset of wrist drop is acute and if there are UMN findings, consider stroke/lesion in hand-knob region of the brain
⊙ CLINICAL PEARL
Weakness can seem more profound in the setting of mechanical disadvantage (e.g. if finger extension is weak, finger abduction may also seem weak since hand is in a "finger drop" position). If finger extensions are weak, place hand on flat surface to examine finger abduction.
Physical exam
Localizing wrist drop:
| Nerve | Sensory changes | Motor weakness | Reflexes affected |
|---|---|---|---|
| C7 | Digit 3 | Pronation of forearm (pronator teres) | Triceps reflex |
| Radial nerve (axilla) | Sensory loss to posterior arm and forearm | Elbow extension (triceps) | Triceps reflex |
| Radial nerve (spiral groove) | Sensory loss in lateral dorsum of hand | Elbow flexion/supination (brachioradialis) | Brachioradialis reflex |
| PIN | N/A | Finger extension weakness: Extension of index finger (EIP), extension of thumb (EPL/EPB), extension of digits (EDC) | N/A |
Investigations
EMG/NCS
+/- CT Head/CTA to rule out stroke for acute wrist drop
Treatment
Symptoms generally resolve in weeks to months
Consider NSAIDs for pain management and wrist splinting to assist with hand function
Common lower extremity mononeuropathies
By Dr. Conrad Eng
Lower extremity anatomy
Nerve roots supplying lumbosacral plexus are L1 - S3
| Nerve | Nerve roots | Muscle innervation |
|---|---|---|
| Femoral | L2-L4 | Iliopsoas, quadriceps |
| Obturator | L2-L4 | Thigh adductors |
| Superior Gluteal | L4-S1 | Gluteus medius/minimus |
| Inferior Gluteal | L5-S2 | Gluteus maximus |
| Sciatic Nerve | L5-S2 | Hamstrings |
| Peroneal Nerve | L4-S1 | Tibialis anterior, peroneus longus/brevis, extensor hallucis longus, extensor digitorum longus/brevis |
| Tibial Nerve | L5-S2 | Gastrocnemius, soleus, tibialis posterior, flexor digitorum longus, flexor hallucis longus |
Lumbosacral Radiculopathy
Pathophysiology
Commonly due to nerve root compression from disc herniation/spondylosis (e.g. degenerative arthritis)
Less common can be due to inflammation, neoplasm, vascular disease
Most common nerve roots affected are L5 and S1
Clinical Features
Lower back pain that is radicular (sharp, burning, needle pain that radiates down leg) with sensory symptoms of numbness, tingling, burning, electric shock
Can also have associated weakness with walking up and down stairs
May have UMN signs
Common tests include straight leg raise (patient supine while examiner raises leg on the affected side with knee extended. Test is positive and suggestive of L5 or S1 nerve root compression if radicular symptoms are reproduced or worsened between 30-70 degrees)
Red flags to rule out for lower back pain
| Symptoms, history | Possible diagnosis |
|---|---|
| Night pain | Tumor |
| Fever, history of recent bacterial infection or IV drug use, severe back spasm | Diskitis or epidural abscess |
| Leg pain | Nerve root compression |
| Bilateral lower extremity weakness or numbness, bladder or bowel dysfunction | Cauda equina or conus compression |
| Major trauma | Fracture, dislocation |
| Minor trauma with osteoporosis | Compression Fracture |
| History of carcinoma | Metastatic disease |
| Systemic symptoms | Multiple myeloma |
| Back pain in child | Tumor, tethered cord |
| Worker’s compensation or legal claim | Secondary gain |
Investigations
MRI lumbar spine +/- GAD
NCS/EMG
Treatment
Improvement over months - a year
Symptomatic treatment with neuropathic pain medications (e.g. pregabalin, gabapentin)
If no improvement or significant pain component - consider referral to pain specialist for epidural injections
If symptoms are significant with motor deficits - referral to surgery
Peroneal Neuropathy
Pathophysiology
Most common lower extremity mononeuropathy
Commonly due to compression against fibular head (leg crossing, trauma, kneeling, surgery, weight loss)
Clinical Features
Motor symptoms include foot drop (due to tibialis anterior) and impairment in foot eversion
Sensory symptoms include numbness along lateral calf and dorsum of foot
Differentiating foot drop
| Nerve | Tibialis Anterior (Ankle Dorsiflexion) | Peroneus longus (Ankle Eversion) | Tibialis Posterior (Ankle Inversion) | Gastrocnemius (Ankle Plantarflexion) | Gluteus medius (Hip Abduction) |
|---|---|---|---|---|---|
| Deep peroneal | X | - | - | - | - |
| Common peroneal | X | X | - | - | - |
| Sciatic nerve | X | X | X | X | - |
| Lumbosacral plexus | X | X | X | * (if S1 involved) | X |
| L5 Root | X | X | X | - | X |
Investigations
NCS/EMG
Treatment
Individualize treatment based on how severe nerve compression is as determined by electrodiagnostic findings
May require orthotics/foot brace to help provide support to the foot with dorsiflexion weakness
Physiotherapy/Occupational therapy to help retrain mobility
Polyneuropathies
By Dr. Caz Zhu
Definition
Affecting multiple nerves - can be classified into polyneuropathy, mononeuropathy multiplex, or generalized neuropathy
Any process affecting the peripheral nervous system that causes pain, paraesthesia, numbness, or weakness
Can affect the nerve roots to the peripheral nerves
**⊙ CLINICAL PEARL **
Unlikely to be a peripheral neuropathy if the patient presents with pure motor symptoms (i.e. absence of pain, numbness, etc)
Clinical Features
What modality is affected? Patients may have numbness, paraesthesia, pain, sensory ataxia, weakness, and autonomic symptoms (e.g. impaired sweating) which may point to one diagnosis more than another
How long has the patient had symptoms? A slower, chronic progression suggests a metabolic, toxic, or genetic (CMT) disease vs an acute onset may be more inflammatory
Length dependent or non-length dependent? Length-dependent patterns are typically axonal and non-length independent are often demyelinating (HOWEVER, demyelination can be associated with axonal loss)
Demyelinating neuropathies are special because acquired demyelinating neuropathies are often treatable
| Axonal | Demyelinating | |
|---|---|---|
| Structure affected | Axonal dysfunction | Myelin affected |
| **Pattern ** | Length-dependent process, ascending from the feet up (glove and stocking) | Proximal and distal involvement, can have hand and feet involvement at the same time |
| Symptoms | Paraesthesia, numbness, commonly vibration/proprioception involvement more than motor involvement | Motor symptoms can be more predominant than sensory symptoms, early loss of reflexes |
| Common etiologies | Metabolic (diabetes, B12, hypothyroidism) , medications, chemotherapy, toxins (alcohol, heavy metals), infections, malignancy, vasculitis | GBS/CIDP, MMN, POEMS, Toxins (amiodarone, chloroquine), Genetics |
Investigations
CBC, ESR, CR, HbA1c, TSH, ANA, B12, SPEP
NCS/EMG
MRI of cauda equina MRI with contrast to assess for root enhancement
+/- LP to send for CSF if concerned for GBS or other immune/malignancy causes
Treatment
Symptomatic treatment for neuropathic pain
** Gabapentin**(Starting dose: 300 mg BID/TID - can increase up to 1800 - 3600 mg max per day), Side effects: Drowsiness, ankle edema, weight gain, and caution in use with patients with renal failure
Pregabalin (Starting dose: 75 mg BID and increase up to 150 - 600 mg max daily) Side effects: Drowsiness
Amitriptyline (Starting dose: 10 mg QHS and increase up to 25 - 50 mg max daily) Side effects: Anticholinergic effects (Drowsiness, constipation, dizziness, dry mouth)
Duloxetine (Starting dose of 60 mg daily and increase to 60 mg BID) Side effects: Nausea, drowsiness, mental fogginess
Treatment of acquired demyelinating disorders
** GBS/CIDP** - See GBS for further information
Patient Education
Importance of foot care, weight loss, management of metabolic and other conditions that is contributing to peripheral neuropathy
Counseling patients that for the majority of peripheral neuropathy (especially metabolic conditions like diabetes), symptoms may not improve or disappear completely even with treatment (success in treating neuropathic pain is 50% reduction in pain in 50% of patients)
Goal of treatment is to help patients live better and help maintain function & mobility (e.g. avoid falling, being able to walk)
Neuro-infectious Disorders
Bacterial Meningitis
By Dr. Jeremy Zung
Reviewed by Dr. Alex Muccilli
Pathophysiology and Epidemiology
Inflammation of meninges - most commonly caused by infection (but can also be caused by chemical irritation, neoplastic causes)
Common pathogens: Streptococcus pneumoniae, Neisseria meningitidis, Haemophilus influenzae, Listeria monocytogenes (immunocompromised, EtOH misuse), Escheria coli
For common bacteria infections per age group, see Figure 1 in the article: Bacterial Meningitis in the United States, 1998–2007
Clinical Features
Fever
Headache
Neck stiffness - may be masked by analgesia or corticosteroids; Kernig and Brudzinski signs (limited sensitivity and specificity)
Altered mental status/level of consciousness
Cranial neuropathies (common with basiliar meningitis)
Seizures
Petechial rash (N. meningitidis)
Infants/children: nausea/vomiting, irritability, lethargy, anorexia, hypotonia, seizures (up to 34%), bulging anterior fontanelle, hydrocephalus
Immunocompromised hosts may not show classic signs!
Investigations
Stat CT head to rule out acute intracranial abnormality (i.e., hemorrhage, stroke, mass lesion) - consider CT with contrast to increase sensitivity for meningeal and parenchymal involvement
CBC
Lytes, extended lytes (Mg, Ca, PO4), creatinine
Blood glucose
Liver enzymes
Toxicology screen if indicated
Blood and urine cultures - bacteremia is common in up to 70% (always do cultures before starting antibiotics)
LP: cell count and differential, protein, glucose, bacterial/viral/fungal cultures and Gram stain, Cryptococcal, VDRL- commonly find leukocytosis (80-90% neutrophils), low glucose, elevated protein in bacteria meningitis
MRI brain with contrast when clinically stable
Consult ID to guide longterm management of antimicrobial agents
Differential for CSF findings
| Neutrophilic pleocytosis | Lymphocytic pleocytosis | Hypoglycorrhachia (CSF: serum glucose less than 0.4) |
|---|---|---|
| Bacterial (not lyme or syphilis), epidural abscess, early viral, early TB/mycobacterial, fungal, cryptococcal, 1° amoebic | Viral (HSV, VZV, CMV), acute HIV, TB, bacterial (syphilis, lyme, leptospirosis,brucella, bartonella), fungal, cancer, partially-treated bacterial meningitis | Bacterial, fungal, carcinomatous, TB, sarcoid, SAH (present in 1%), lymphoma/carcinomatosis |
Treatment
If there is a strong suspicion for meningitis and the patient is unwell (e.g. decreased level of consciousness) , do not wait to do a lumbar puncture to start empiric antibiotics (rapid start of antibiotics is crucial to decrease mortality)
Empiric treatment: CTX 2g IV BID or Cefotaxime 2g IV q4-6h + Vancomycin 1-2g IV q12h + Dexamethasone 10mg IV q6h (x 4 days) (administered before or with first dose of antibiotics + Acyclovir 10mg/kg IV q8h (as it is difficult to exclude viral encephalitis)
Consider adding Ampicillin 2g IV q4h if patient is less than 2, older than 50, immunosuppressed, or chronically ill for Listeria coverage
Steroids are associated with reduced risk of hearing loss in children, and reduced morbidity/mortality with S. pneumoniae
Antimicrobial therapy can be adjusted depending on cultures
| Organism | Antimicrobials | Duration of Treatment (days) |
|---|---|---|
| S. pneumoniae | CTX 2g IV BID or Cefotaxime 2g IV q4-6h + Vancomycin 1-2g IV q12h + Dexamethasone 10mg IV q4-6h | 10-14 |
| N. meningitidis | CTX 2g IV BID or Cefotaxime 2g IV q4-6h | 7 |
| H. influenzae | CTX 2g IV BID or Cefotaxime 2g IV q4-6h | 7-10 |
| L. monocytogenes | Ampicillin 2g IV q4h | 21 |
| P. aeruginosa | Meropenem 2g IV q8h or Ceftazadime 2g IV q8h + Vancomycin 1-2g IV q12h | 21 |
Patient Monitoring
There are increased risks of hearing loss, cognitive impairment, hemiparesis, epilepsy, vasospasm, ischemic and hemorrhagic stroke, and cerebral venous thrombosis
Patient Education
Patients at risk should receive Prevnar vaccinations to reduce the risk of bacterial meningitis due to S. pneumoniae
Neurosyphilis
By Dr. Jeremy Zung
Reviewed by Dr. Alex Muccilli
Clinical Features
Primary - mean 2-3 weeks post-exposure; spontaneous resolution within 3-6 weeks without treatment
Chancre: painless, non-pruritic, genital or oral
Lymphadenopathy
Secondary - mean 2-12 weeks post-exposure but can occur over weeks-years and resolve without treatment; early neurosyphilis
Rash: diffuse, symmetric, macular including palms/soles, condyloma lata in intertriginous regions and mucous patches
Neurological features: meningitis/encephalitis, meningovascular syphilis causing stroke (10%), cranial nerve palsies (especially II, III, VI, VII), uveitis/iritis with decreased visual acuity, otosyphilis with hearing loss and tinnitus, behavioural/cognitive changes
Other organ involvement: hepatitis, nephropathy, adenopathy, fever, sore throat, headache, generalized painless lymphadenopathy
Tertiary - years-decades post-exposure; late neurosyphilis
Cardiac involvement: aortitis, aortic aneurysms, saccular aneurysms
Gummatous lesions: affect long bones, upper respiratory tract
Neurological features: Symptoms of early neurosyphilis, PARESIS (see table below), and tabes dorsalis (33% - affects dorsal roots and dorsal columns of spinal cord)
| PARESIS | Features |
|---|---|
| Personality disturbances | Mania, Psychosis |
| Affect abnormalities | Depression |
| Reflex hyperactivity | |
| Eye abnormalities | Uveitis/keratitis, Argyll Robertson pupils (constrict to accommodation but not to light, irregular pupil - Video) |
| Sensory changes | Sensory loss, impaired vibration and proprioception, lancinating pain, sensory ataxia |
| Intellectual impairment | Fronto-temporal dementia |
| Slurred speech |
Latent - asymptomatic period
Investigations
| Investigations | ||
|---|---|---|
| Serum nontreponemal tests | Venereal disease research laboratory (VDRL), Rapid plasma reagin (RPR). | |
| Serum treponemal tests | Fluorescent treponemal antibody absorption (FTA-ABS)., T. pallidum particle agglutination assay (TPPA)., T. pallidum enzyme immunoassay (TP-EIA) and chemiluminescence immunoassay (CIA) | *NOTE: Public Health Ontario uses this chemiluminescent microparticle immunoassay as a first screen, then confirms with RPR or TPPA. |
| CSF | Lmphoytic pleocytosis, elevated protein, CSF VDRL |
If serum assays are positive:
If reactive and symptoms/signs are consistent with neurosyphilis, then perform lumbar puncture with CSF-VDRL. If positive, then treat for neurosyphilis.Even with CSF-VDRL negative, treat for neurosyphilis if any abnormalities in CSF e.g. >5 WBC/microL or protein >0.45g/L and high clinical suspicion.
Treatment
Penicillin G 4 million units IV q4h x14 days.
Jarisch-Herxheimer reaction: result of release of endotoxin-like products within a few hours of the first dose of antibiotic; fever, chills, hypotension, hyperventilation, flushing.
If Penicillin allergy: Ceftriaxone 2g IV daily x14 days.
If severe Penicillin allergy: Doxycycline 200mg p.o. BID x28 days.
Patient Education
Pregnancy: screening (e.g. CIA) should be performed at the time pregnancy is confirmed.
Serologic and CSF titres of VDRL can be checked and fall with treatment of syphilis.
If untreated, syphilis can lead to tabes dorsalis or general paresis of the insane (frontotemporal dementia), which have declined in the antibiotic era.
Neuro-otology
Reviewed by Dr.Tess Fitzpatrick
The Head Impulse-Nystagmus-Test of Skew (HINTS) exam is a useful test to assess for central vs peripheral causes of vertigo/gait unsteadiness.
Head Impulse: Testing vestibulo-ocular reflex (VOR) by having the patient maintain focus on the examiner’s nose while the examiner quickly turns the patient’s head sharply to left or right (caution: avoid if patient has a cervical spine injury or vessel dissections) - abnormal head impulse is characterized by a re-fixation saccade (eyes will look away and then back at examiner's nose) and is suggestive of peripheral vertigo - Video demonstration of abnormal head impulse test
Nystagmus: Assessing if patient has nystagmus in primary gaze or looking in different directions, what kind of nystagmus it is (horizontal, vertical, torsional, direction-changing) - any nystagmus that is NOT unilateral or dominantly horizontal is concerning for a central lesion - Video demonstration of vertical nystagmus
Skew deviation: Misalignment of eyes - alternate-cover test while patient fixates on a distant target and see whether there is vertical movement of the eyes; presence of skew deviation suggests central lesion - Video demonstration of skew deviation
| Central Vertigo | Peripheral Vertigo | |
|---|---|---|
| Head Impulse | Normal, no corrective saccades | Abnormal with head turning, corrective saccades back to midline when head is turned |
| Nystagmus | Vertical, Horizontal & direction-changing, Torsional | Unidirectional, dominantly horizontal (can have some mixed horizontal/torsional component) |
| Test of skew | Skew deviation present | No skew deviation |
Benign paroxysmal positional vertigo (BPPV)
By Dr. Kia Gilani
Reviewed by Dr.Tess Fitzpatrick
Pathophysiology
Irritation of semicircular canals due to otoliths - usually induced by sudden change in head position (e.g. turning over in bed)
Most commonly affected semicircular canal is posterior (followed by anterior and horizontal)
Clinical Features
Acute onset vertigo (“the room is spinning”, “I’m on a rocking boat”) provoked by head movements and can be associated with nausea/vomiting
Can have multiple episodes that are short-lasting (< 1 minute) but due to periods of feeling unwell in between, patients often report that their symptoms are constant
Differential Diagnosis
| Clinical features | Distinctive from BPPV | |
|---|---|---|
| Meniere’s Disease | Episodic attacks of vertigo with fluctuating hearing loss, aural fullness, and tinnitus in affected ear,triggered by head position changes, nausea/vomiting present | Vertigo symptoms can last hours (instead of seconds-minutes like BPPV) |
| Vestibular neuritis | Acute onset vertigo (often due to viral prodrome) - with vestibular labyrinthitis, can also have hearing loss/tinnitus | Vertigo is gradual onset (developing over hours), sustained, can occur at rest and can last days-weeks |
| Central cause (e.g. posterior circulation stroke, demyelination) | Acute onset vertigo with other neurological symptoms (gaze palsies, ataxia, dysarthria, nystagmus) | Vertigo symptoms are constant and sustained |
Investigations
Diagnosis is made with a positive Dix-Hallpike test (DHT): Bring patient from upright to supine with head turned 45 degrees to one side and neck extended 20 degrees and look for vertigo and upbeating and torsional nystagmus. Repeat this with the head turned towards the opposite direction, if no nystagmus is elicited - Video demonstration of Dix-Hallpike
CAUTION: If downbeat nystagmus appears → consider central etiology
Treatment
Monitor - At least 30-50% of cases will resolve spontaneously without any treatment
Epley maneuver - Video demonstration of Epley
Vestibular rehab especially if there is a heightened risk of falls
Pharmacotherapy generally not effective but helpful for symptomatic management/prophylaxis prior to repositioning maneuvers but not for resolution of symptoms (e.g. antihistamines (diphenhydramine), betahistine, ondansetron)
Patient Education
Recurrence of symptoms is common (up to 30%) so important to counsel patients that symptoms may return/reoccur
Patients can access www.vestibular.org for resources
Neuro-ophthalmology
Anterior Ischemic Optic Neuropathy (AION)
Clinical Features: Two forms of AION- Non-arteritic AION (NAION) and Arteritic AION (AAION), which is typically caused by GCA.
Cranial Nerve III (oculomotor) Palsy
By Dr. Kia Gilani
Reviewed by Dr. Jonathan Micieli
**Anatomy **
The oculomotor (CN III) nuclear complex is in the midbrain at the level of the superior colliculus. It is ventral to the sylvian aqueduct, and dorsal to the medial longitudinal fasciculi
Innervates superior rectus, medial rectus, inferior rectus, and inferior oblique - Elevation, depression, and adduction of the eye
Innervates levator palpabrae - Eyelid elevation
Edinger-westphal nucleus is posterior to CN III - supplies parasympathetic fibers for pupil constriction
Click image to enlarge
Clinical Features
Complete palsy: Ptosis, large unreactive and dilated pupil, paralysis of eye adduction, elevation, and depression
**Partial palsy: **Variably affect pupil, eyelid, and involves extraocular muscles
**Pupil-sparing CN III : **Pupillary fibers run on the medial exterior part of the nerve while the oculomotor fibers are inside the nerve. Thus, most compressive lesions will affect the pupillary fibers (causing impaired pupillary constriction) compared to ischemic lesions that affect the innermost fibers and often spares the pupil
Aberrant Regeneration: Indicative of chronic CN III palsy, with regeneration of axons that results in unintended ocular findings with attempted movement - may be suggestive of tumor, aneurysm, or trauma (can be seen by elevation of eyelid with downward gaze or adduction of the eye)
Left CN 3 Palsy (Click image to enlarge)
Source: Case-based neuro-ophthalmology
Differential Diagnosis
Majority of patients >50 with isolated CN III palsy have microvascular cause
BUT MUST RULE OUT aneurysmal etiology
| Microvascular | Aneurysmal |
|---|---|
| Most common cause, seen in patients over 50 years with vascular risk factors | Neurological emergency - associated commonly with PCOM aneurysm (but can also be basilar or cavernous sinus carotid aneurysm) - risk of subarachnoid hemorrhage |
| Acute or subacute, progressive over 2-4 weeks but should resolve by 3 months. If no recovery, than consider alternative diagnosis | 78% have pain/headaches |
| Patients may present with headache and eye pain | Always has pupillary involvement (dilated, non-reactive pupils) |
**Other etiologies **
Trauma - most common cause in young people and can occur post-neurosurgical procedure
Compression due to malignancy, sellar masses (e.g. pituitary apoplexy, pituitary adenoma)
GCA - may present as cranial neuropathy, do ESR/CRP
Neuromuscular (Myasthenia Gravis, Miller-Fisher)
Congenital
Physical Exam
Testing for extraocular movements, pupils, and convergence
Misalignment can be comitant (deviation similar to all position of gazes), or incomitant (deviation differs depending on gaze position).- childhood strabismus is comitant
Investigations
Blood pressure, glucose, HbA1c, ESR, CRP, platelets
CT/CTA (for all patients to rule out aneurysms)
If pupil is normal: Observe, no MRI in the beginning
If pupil is abnormal: URGENT MRI Brain with Orbits with GAD to rule out aneurysm or compressive lesion
Treatment
Aneurysm - Should be assessed by neurosurgery for consideration of endovascular coiling or surgical clipping (63% of patients with PCOM aneurysms operated on within 2 weeks of onset made complete recovery, compared to 30% 2-4 weeks, and 17% >1 month)
Ischemic/Microvascular cause - Usually conservative treatment including patching, prisms. Ocular surgery may be helpful to restore primary position alignment if CN III palsy persists
Click image to enlarge
Patient Education
Microvascular palsy: A vast majority of patients with microvascular third nerve palsy have complete recovery. Complete recovery is less common in post-neurosurgery (36%), aneurysmal (33%) and neoplastic (19%) compressive, and traumatic (22%).
Aneurysmal palsy: with successful aneurysm treatment a majority of patients have complete or partial recovery, which can take up to a year
Cranial Nerve IV (Trochlear) Palsy
By Dr. Kia Gilani
Reviewed by Dr. Jonathan Micieli
**Anatomy **
The trochlear nerve (CN IV nerve) is caudal to CN III, dorsal to MLF at the level of the inferior colliculus
The only nerve that runs dorsally from the brainstem
Innervates the superior oblique muscle - eye depression
Click image to enlarge
Clinical Features
CN IV Palsy causes hypertropia and excyclotorsion of the affected eye and patients may complain of vertical or horizontal diplopia
Hypotropia seen in the normal eye when the affected eye is fixating
Hypertropia is seen in the affected eye when the unaffected eye is fixating
Presence of excyclotropia
Patients may develop head tilt to compensate for hypertropia and cyclotropia (usually away from affected side)
The Three Step Test helps identify the CN IV palsy
Step 1: Identify hypertropic eye (the eye that looks higher up)
Step 2: Identify gaze direction which worsens hypertropia. Adduction of hypertropic eye should increase hypertropia if there is a CN IV palsy.
Step 3: Identify direction of head tilt that increases hypertropia
Example: For a LEFT CN IV palsy, the LEFT eye will be hypertrophic, looking RIGHT would worsen hypertropia, and tilting the head LEFT worsens hypertropia (Many patients will tilt their head on the opposite side of the CN IV palsy to compensate and improve their diplopia )
Left CN 4 Palsy (Click image to enlarge)
Source: Case-based neuro-ophthalmology
Differential Diagnosis
| Microvascular | Traumatic | Congenital | Intracranial lesions |
|---|---|---|---|
| Most common especially in patients older than 50 with diabetes/vasculopathic risk factors and often resolves without neuro-imaging. However, if progressive, associated with other neurological symptoms or not resolving within several months, may require imaging. | Most common cause of isolated/bilateral CN IV lesions, imaging may help identify structural lesion | Assess old photos for head tilt, have cyclotropia on exam but no torsional diplopia | Rarely isolated CN IV, usually with other neurological symptoms |
Investigations
Blood pressure, glucose, HbA1c, CBC
If > 50 - ESR/CRP
If other CN involvement and not congenital/traumatic - Consider MRI brain and orbits with contrast
Treatment
Non-pharmacological: Prisms and occasionally occluding one eye for symptomatic relief
Strabismus surgery: Indicated if lack of spontaneous improvement in 6 months
(Click image to enlarge)
Patient Education
Spontaneous improvement in 44% of patients from traumatic CN IV palsy (few days - months)
Majority of patients with microvascular CN IV palsy improves by 4-6 months
If no improvement after 6 months, consider corrective surgery
Cranial Nerve VI (Abducens) Palsy
By Dr. Kia Gilani
Reviewed by Dr. Jonathan Micieli
Anatomy
The abducens (CN VI) nucleus is located in the dorsal lower pons, separated from the floor of the 4th ventricle by the facial nerve fascicle (facial colliculus)
Innervates the lateral rectus - Abducts the eye
Coordinates horizontal eye movements (Looking to the right - right eye ABDUCTS and left eye ADDUCTS) - CN VI motor neurons are mixed with internuclear neurons through the medial longitudinal fasciculus (MLF), ascending through the pons and midbrain, terminating in the oculomotor (CN III) nucleus - Internuclear Opthalmoplegia (INO) can be a result if MLF is damaged
Click image to enlarge
Clinical Features
CN VI Palsy causes impaired abduction of the eye, horizontal diplopia and eso-deviation of the eye that is worse upon attempted abduction of the affected eye
Right CN 6 Palsy (Click image to enlarge)
Source: Case-based neuro-ophthalmology
Differential Diagnosis
| Etiology | Ischemic | Masses//Raised ICP | Congenital |
|---|---|---|---|
| Differential | Diabetes, collagen vascular disease, giant-cell arteritis, parainfectious or post-infectious vasculitis | Skull-based or sellar masses (e.g. pituitary adenoma, ICA aneurysm) , idiopathic intracranial hypertension, CVST | Mobius syndrome |
| Associated Signs & Symptoms | Pain with eye abduction, headache, scalp tenderness, jaw claudication | Visual acuity loss, papilledema, headaches | Facial diplegia and other cranial nerve abnormalities, bilateral ocular abduction weakness and conjugate horizontal gaze paresis |
Other causes can include trauma, demyelination, inflammatory (neurosarcoid), or idiopathic
Investigations
If papilledema present - urgent MRI with contrast
Bloodwork: Blood pressure, glucose, HbA1c, ESR, CRP
Patients with isolated CN VI palsy that are >50 years of age, with microvascular risk factors (diabetes, hypertension) may not require neuroimaging
If patients do not improve in 3-4 months, consider MRI Brain with Orbits with GAD
Treatment
First 6 months: Patching and botulinium toxin injections may improve diplopia. Many CN VI palsies resolve within several months, and symptomatic management is warranted
>6 months: If CN VI palsy does not improve by 6 months, surgery is indicated
Patient Education
The importance of follow up must be discussed with patients that are not undergoing neuroimaging. Follow-up in 10-12 weeks after onset, lack of improvement may warrant imaging
Microvascular: 62% of patients recover over 6 months
Traumatic: Traumatic CN VI palsies recovery in almost all cases if partial, and in 1/3 of cases if complete
Idiopathic: A majority of patients with undetermined cause recover CN VI function
Optic neuritis
By Dr. Kia Gilani
Reviewed by Dr. Jonathan Micieli
Pathophysiology and Epidemiology
Typically in people in their 30’s, 77% female
Most commonly seen in demyelinating diseases - e.g. multiple sclerosis, NMOSD/MOG
Clinical Features
Features of Optic Neuritis include:
Must have RAPD (unless bilateral involvement)
Acute or subacute eye pain (or pain with eye movements)
Vision loss or blurry vision - typically peaks in 1-2 weeks
Dyschromatopsia and contrast sensitivity loss - abnormal color vision
Absent or mild disc edema
Red flags suggestive of a diagnosis outside of optic neuritis (additional testing may be required)
Age >50
Painless vision loss
Retinal abnormalities
Severe vision loss without early recovery
History of cancer
Worsening visual function after reducing or stopping steroids or immunosuppressants
| Findings | Typical ON | Atypical ON |
|---|---|---|
| Characteristics | Unilateral, Pain with extraocular movements, RAPD, Gradual vision loss | Unilateral and/or bilateral, Recurrent episodes, Gradual and/or acute visual loss, Typically younger than 12 and older than 55 year old patients |
| Fundoscopy | Absent or mild disc edema, Absence of intraocular inflammation, Absence of optic disc hemorrhages, retinal hemorrhages, or retinal vasculitis | Optic disc edema, Additional features including intraocular inflammation, hemorrhages, or retinal vasculitis |
| Associations | Multiple sclerosis | NMOSD, Lyme, TB, VDRL, HIV, sarcoidosis, vasculitis |
| Prognosis | Recovery of vision without treatment, | No recovery without treatment and/or progression of visual symptoms, Relapse after steroid withdrawal |
Investigations
Patients should have a visual acuity measurement, retinal exam, clinical and formal visual field testing including red desaturation, pupil examination looking for RAPD.
Bloodwork: CBC, ESR/CRP, VDRL, ACE, ANA
NMO/MOG serum antibodies
MRI Brain and Orbits with GAD
Consider additional work-up including a lumbar puncture (CSF: Cytology, protein, glucose, oligoclonal bands)
Treatment
Acute treatment: IV Methylprednisolone or PO high-dose steroids
ONTT study found IV methylprednisolone accelerates visual recovery but no benefit in visual acuity at 2 years
Dose and Duration: Methylprednisolone 1000 mg IV or Prednisone 1250 mg PO for 5 days
For atypical cases that do not improve after initial treatment: consider prednisone 1 mg/kg pulse
Adverse effects: Sleep disturbance, mood changes, weight gain, GI irritation, avascular necrosis
Patient should also be on Vitamin D and Calcium
Other acute treatments: PLEX for steroid resistant severe optic neuritis
Long term management: If a diagnosis of a demyelinating disorder (e.g. MS) is suspected, patient should be referred to for consideration of disease modifying therapies
Click image to enlarge
Non-Anterior ischemic optic neuropathy (NAION)
By Dr. Andrea Kuczynski
Reviewed by Dr. Jonathan Micieli
Pathophysiology and Epidemiology
Idiopathic, vascular insult due to transient hypoperfusion of the optic nerve head
Does not involve embolic infarction
Common in middle aged individuals; more common in Caucasians due to smaller cup-to-disc ratios
Risk Factors
Vascular risk factors: HTN, dyslipidemia, type II diabetes, ischemic heart disease, OSA, tobacco use, nocturnal hypotension, coagulopathies
PDE5 inhibitors (e.g., Viagra, Tadalafil)
Renal failure on dialysis
Optic disc drusen
Clinical Features
Acute, painless, monocular vision loss
Ocular pain (present in 10%)
Disc-at-risk (unaffected optic disc is at risk of optic disc edema) - essential for the diagnosis
Fundoscopy: disc edema (may persist for 6-11 weeks), pallor, may see peripapillary wrinkles caused by displacement of the retina by the disc edema
Diagnosis is made when the disc edema resolves within the appropriate time course
Investigations
CBC
ESR/CRP
Monitor BP and avoid hypoperfusion which can exacerbate
Referral to Ophthalmology/Neuro-ophthalmology
Treatment
None - may have mild to no improvement in vision
Treatment of vascular risk factors in an attempt to preserve visual function in the other eye
Patient Education
Management of vascular risk factors (compliance with medications, CPAP if OSA present) is important to protect the unaffected eye
15% of patients risk development of NAION in the other eye at 5 years
Neuroretinitis
By Dr. Andrea Kuczynski
Reviewed by Dr. Jonathan Micieli
Pathophysiology and Epidemiology
Inflammatory condition of the optic disc vasculature resulting in disc edema
Risk Factors and Causes
Infections: VDRL, TB, Lyme, WNV, Toxoplasmosis, Bartonella (most common; “cat scratch disease”)
Parainfectious: MMR, HSV/VZV, EBV, CMV, coxsackie B
Inflammatory: sarcoidosis, IBD, polyarteritis nodosa, tubulointerstitial nephritis and uveitis
Clinical Features
Acute, painless, monocular vision loss
RAPD if unilateral
Fundoscopy: disc edema, macular edema, macular exudates (“macular star”; late finding), subretinal fluid, loss of architecture under the fovea
Macular star pattern (Click image to enlarge)
Source: Case-based neuro-ophthalmology
Investigations
Referral to Ophthalmology/Neuro-ophthalmology
CBC
ESR/CRP
Infectious work-up: VDRL, Bartonella serology, Toxoplasmosis serology, and additional serology if indicated depending on clinical history
CXR
MRI brain with orbits (typically normal)
Treatment
None - most patients have gradual resolution without treatment
Antimicrobials depending on etiology (i.e., Azithromycin for cat scratch disease, Penicillin G for VDRL)
central retinal artery occlusion / Branch retinal artery occlusion (CRAO and BRAO)
By Dr. Andrea Kuczynski
Reviewed by Dr. Jonathan Micieli
Pathophysiology and Epidemiology
Vascular insult due to transient hypoperfusion of the optic nerve head typically due to vasculitic or embolic cause
CRAO is less common than BRAO
Common in middle aged individuals
Risk Factors
Vascular risk factors: carotid artery atherosclerosis, HTN, dyslipidemia, type II diabetes, ischemic heart disease, OSA, tobacco use, nocturnal hypotension, coagulopathies
Cardioembolic risk factors (more common in patients <40-years-old): infective endocarditis, IVDU, rheumatic heart disease, cardiac tumor
Other vascular disease: fibromuscular dysplasia, carotid artery dissection, Moyamoya disease, Fabry disease
Inflammatory disease: GCA, vasculitis, Susac syndrome, sarcoidosis
Clinical Features
Acute, painless, monocular vision loss
CRAO typically has more severe vision loss, rarely can count fingers but can identify hand motions
BRAO has less severe vision loss usually restricted to part of the visual field
Associated symptoms depending on etiology: headache, jaw claudication, unilateral sensory-motor loss, neck pain
Fundoscopy: ischemic retinal whitening, cherry red spot, retinal emboli (up to 40% of patients with CRAO)
Fluorescein angiography: slowed or absent filling of the central retinal artery with sparing of the choroid in the acute phase; if the choroid is also affected, consider GCA
Investigations
Can be seen as a Code Stroke - CONSULT OPHTHALMOLOGY STAT IF NOT ALREADY INVOLVED
CBC
ESR/CRP
Stroke work-up: HbA1c, Lipids, Echocardiogram, Holter monitor 48hrs, Referral to TIA/Rapid Stroke Clinic or ED (if patient seen in peripheral site/clinic)
Ophthalmology/Neuro-ophthalmology consultation/referral ASAP for fundoscopy and visual field testing
MRI/MRA brain and neck vasculature (or CT/CTA to obtain images quicker)
Treatment
Antiplatelet agent if no contraindications (i.e., already fully anticoagulated for another reason)
Treatment of vascular risk factors in an attempt to prevent recurrence and preserve visual function
Requires Ophthalmology to follow after the initial presentation to monitor for neovascular complications
Patient Education
Management of vascular risk factors (compliance with medications, CPAP if OSA present) is important to protect visual function
BRAO has a much better prognosis than CRAO, with up to 80% of patients recovering visual function; CRAO has a poor prognosis for spontaneous visual recovery
Arteritic Anterior ischemic optic neuropathy (AAION)
By Dr. Kia Gilani
Reviewed by Dr. Jonathan Micieli
Pathophysiology and Epidemiology
For those > 50, must consider Giant Cell Arteritis (GCA) in the differential diagnosis
Most common in females and Caucasians of Scandanavian descent
GCA can be associated with Polymyalgia Rheumatica (proximal muscle pain and stiffness that is worse in morning)
Differential Diagnosis
Giant Cell Arteritis
ANCA-associated vasculitis
Infection
Neoplastic
Clinical Features
Sudden, profound visual loss that can become bilateral in hours to days
Diplopia - Transient or persistent
Majority of patients have systemic symptoms: (Headache, scalp tenderness, jaw claudication, muscle aches/stiffness in the morning, malaise, fever)
Superficial temporal artery pulse: Cord-like feel with reduced pulses
Fundoscopy: optic disc may appear swollen, pale “chalky white” optic nerve head with nerve fiber layer hemorrhage and cotton wool spots
Fundoscopy of GCA (Click image to enlarge)
Source: Case-based neuro-ophthalmology
American College of Rheumatology Diagnostic Criteria for GCA
Minimum of 3 criteria from the following:
Age at onset ≥ 50 years
New headache
Temporal artery abnormality: tenderness or reduced pulsation
ESR ≥ 50 mm/hour
Abnormal artery biopsy demonstrating vasculitis, with mononuclear cell or granulomatous inflammation
Investigations
CBC
MUST DO ESR AND CRP
Referral to Ophthalmology/Neuro-ophthalmology and Rheumatology
MRI brain and orbits with GAD
If high pre-test probability of GCA: Consider temporal artery biopsy
Treatment
Confirmed GCA - Steroid pulse (do not delay for temporal artery biopsy because it can lead to permanent vision loss)
Methylprednisolone 1g IV pulse for 3-5 days with subsequent taper of with PO prednisone; in some cases of GCA, can treat with Prednisone 1 mg/kg dosing
Adverse effects: Sleep disturbance, mood changes, weight gain, GI irritation, avascular necrosis
Patients should also be on Vitamin D and Calcium
Patient Education
Vision loss at time of presentation may be irreversible but steroids can prevent further progression
Neurocritical care
TWH Level 2 ICU guide
By Dr. Andrea Kuczynski and Dr. Caz Zhu
Reviewed by Dr. Shaurya Taran, Dr. Leanne Casaubon, Tim Stewart, Dr. David Chan, and Dr. Jane Liao
How to use this guide
This guide was created to help residents feel more comfortable with managing the Level 2 during their neurology - stroke rotation at Toronto Western Hospital. This is meant to be a quick resource for different situations a resident may experience during the day or on call.You should always promptly go and assess a patient for whom you’ve been called for a change in clinical status. You should always document your assessment and plan before the end of the shift.
Consider calling CCRT if patients show acute changes in:
Airway - Threatened airway, stridor, excessive secretions (with vital sign changes)
Breathing - Respiratory rate > 30 or < 8, Oxygen saturations < 90% on 6L/min, or respiratory distress
Circulation - sBP < 90 mmHg or > 200 mmHg (if patient symptomatic) or changes of sBP > 60 mmHg
Disability - Altered Mental Status
You should ALWAYS call CCRT if you have concerns about a patient
Always call your staff if a patient becomes sick (e.g. status epilepticus, blown pupil)
or if you need to administer emergency medications
Change in Medical Status
Examples: Change in level of conciousness/behaviour, vital signs (e.g. fever) abnormalities, patient-specific concerns (e.g. chest pain)
Investigations: STAT CBC, lytes, extended
lytes, Cr, blood glucose, lactate, troponin,
VBG
+/- STAT blood cultures x 2 and urine
cultures
+/- STAT CXR and/or ECG
+/- STAT Imaging based on context
+ Check for good IV access
Call CCRT and staff if concerned
Change in GCS or NIHSS
1. Assess the patient to confirm GCS/NIHSS change
2. Consider STAT CT Head if patient stable
3. Consider possible etiologies:
New stroke (re-infarction, new territory infarct,
hemorrhagic conversion)
Medications/drugs (check medication history for opioids, benzos)
Metabolic derangements (lytes, extended lytes, glucose, lactate)
Infection
Structural causes (hematoma expansion, edema, bleed)
Post-ictal
Symptomatic hemorrhagic conversion
Symptomatic hemorrhagic conversion
1. Investigations: STAT CBC, PTT/INR
2. Early blood pressure management (See Blood Pressure Targets section)
3. Hold DVT prophylaxis and antiplatelets/anticoagulants
4. Review case with staff MD
5. Repeat CT Head if patient clinically deterioates
Patient with acute onset fixed, dilated pupil
(“blown pupil”) and change in LOC
1. Call Code Blue +/- CCRT (if not protecting airway or GCS < 8)
2. Call RT for hyperventilation
3. Keep patient’s head of bed (HOB) > 30 degrees
4. Ensure you have IV access & avoid hypotension
5. Consider hyperosmolar solution and speak to ICU:
Hypertonic saline: 150-300 cc bolus over 15 - 30 min (Useful if patient needs volume expansion, Avoid if Na > 160)
20% mannitol (1 – 1.5 g/kg BOLUS over 10-15 mins) * Rough calculation: patient wt in kg x 5 = amount of mannitol in mL to infuse (Useful if patient needs diuresis, Avoid mannitol in hypotension, poor renal function, or serum osmolality > 320 + Ensure patient has a foley in situ)
6. Call for STAT CT Head once patient stable and call
Neurosurgery if not already involved
Status Epilepticus
See Status Epilepticus section
Blood Pressure Targets
These targets can vary case by case! Please use the standardized order sets for post-tPA/EVT for blood pressure parameters
**Ischemic stroke not eligible for tPA/EVT ** – Permissive hypertension if sBP < 220 mmHg (If sBP > 220 mmHg or dBP > 120 mmHg, then reduce blood pressure by 15-25% over the first 24 hours
Ischemic stroke pre-tPA – BP < 180/105 mmHg (For stroke at UHN, otherwise 185/110)
**Ischemic stroke post-tPA ** – BP < 180/105 mmHg
Ischemic stroke post-EVT – sBP < 180/105 mmHg (Please check with stroke and INR staff for targets
Intracerebral hemorrhage – sBP < 140 -160 mmHg (Aim to reach sBP < 140 mmHg in 1-2 hours especially if spot sign positive, Factors that favor sBP <140 mmHg: LSN < 6 hours, initial sBP < 220 mmHg, anticoagulants, no renal dysfunction, spot sign positive on CTA)
Blood Pressure Management
Remember to repeat/cycle blood pressure regularly
when you’re giving medications!
Hypertension
1. Address underlying cause (e.g. pain, agitation, missed drugs, urinary retention, new stroke/hemorrhage)
2. Consider if patient requires immediate (IV) or gradual (PO/NG) treatment
* based on TORBSST +/- SLP assessment
Immediate: Acute ischemic stroke, acute ICH
Gradual: Non-emergent scenarios
Medications for Hypertension
1. Labetalol 10-20 mg IV push over 1- 2 mins (q10min PRN)
Max total dose 150 mg if received tPA
Max total dose 300 mg if no tPA
AVOID: HR < 50
2. Hydralazine 5-20 mg IV push over 1 - 2 mins (q15-20min PRN)
CAUTION: Unpredictable response, can cause sudden
drop in BP and can cause rebound HTN
Max dose: 40-50 mg q4hrs
3. Enalapril 1.25 mg IV x 1 over 5 mins
Hypotension
In acute stroke post-tPA, avoid pressor support as there is
increased risk of secondary ICH (Level A evidence)
1. Address underlying cause (medications, sepsis,
cardiac, PE)
2. +/- IV fluids and hold antihypertensives, opioids
3. Investigations dependent on likely cause: ECG, troponin, lactate, +/- blood cultures/imaging
if concerned about sepsis: Fluids and antibiotics
if concerned about cardiogenic/PE: Call CCRT or Cardiology
4. Give fluid bolus & hold anti-hypertensives
5. Consult ICU if pressor support required
Rhythm Abnormalities
Tachyarrhythmia (or atrial fib)
Unstable (ischemic chest pain, acute heart failure, sBP < 90, altered LOC):
1. CCRT - for cardioversion
2. Order STAT ECG, CXR, troponin, lytes, extended lytes
Stable: (failed TORBSST)
1. Order lytes, extended lytes
(target Mg > 1, K > 4), troponin, CXR, ECG
2. Give metoprolol 2.5 – 5 mg IV push over 1-2 minutes (q5min, can give up to 3 doses)
CAUTION: Hypotension, bradycardia, acute heart failure. Must be by patient’s bedside if you are giving this on the ward (cycle blood pressure q2-5 minutes)
3. If patient becomes hypotensive - consider fluid bolus (ensure no heart failure on
recent echo)
Bradyarrhythmia
Unstable (ischemic chest pain, sBP < 90, altered LOC):
1. CCRT - transcutaneous pacing
2. Order STAT ECG, CXR, troponin
Stable:
1. Telemetry (if patient is not in Level 2), hold AV nodal agents (Beta blockers, Calcium channel blockers, Digoxin), order TSH/echo/serial troponins
2. Keep atropine 1 mg IV at the bedside in case HR < 40 and hypotensive (Atropine 0.5 mg IV push q3-5min | Max dose: 3 mg)
Level 2 Infusion Orders
Indications: Varies case by case; can be used if requiring frequent prns (e.g q1-2h) or tight blood pressure targets (e.g. sBP 110 - 140)Hypertension
Labetolol 0.125 - 3 mg/min with sBP range _ to _ (typically start at 1 mg/min)Hypotension
Levophed 0.02 - 0.35 mcg/kg/min with sBP range _ to _CAUTION: If patient is persistently hypotensive requiring levophed - call ICU
Coma & Brain Death
By Dr. Andrea Kuczynski
Definitions
Alert: normal state of arousal
Obtunded: loss of responsiveness to some stimuli but still able to communicate
Stupor: only arousable to vigorous, repetitive stimuli with inability to communicate
Coma: unarousable, unresponsive individual with reflexes present
Brain death: comatose patient without intact reflexes
(Click image to enlarge)
[Source: The ICU book - Paul Marino 2013]
Herniation Syndromes
Uncal: inner portion of the temporal lobe is pushed down causing lateral deviation and pressure onto the midbrain; commonly compresses CN3 and motor tracts resulting in a unilateral dilated pupil and ipsilateral hemiparesis (Kernohan’s phenomenon)
Central: due to lesions higher up in the brain causing downward pressure and deviation through a notch in the tentorium; causes small, equal pupils (early) to mid-position fixed pupils (late), bilateral Babinski response, and decorticate posturing
Subfalcine: subfalcine compression under the falx; often presenting with contralateral leg weakness and frontal behavioural changes, or asymptomatic in the majority
External: common in cases of malignant MCA syndrome/edema
Upward: due to infratentorial ischemic/hemorrhagic events or mass lesions with edema resulting in cerebellar (i.e., nystagmus, ataxia) and brainstem signs (i.e., respiratory changes, obtunded state)
Tonsillar: compression of the medulla due to cerebellar tonsil herniation through the foramen magnum; often presenting with medullary signs (i.e., Cheyne-Stokes respiration to respiratory arrest) and Cushing’s reflex (widened pulse pressure, bradycardia, hypertension)
(Click image to enlarge)
Investigations
Stat CT head to rule out intracranial cause (i.e., stroke, hemorrhage, mass lesion)
CBC
Lytes, extended lytes (Mg, Ca, PO4), creatinine
Blood glucose
Liver enzymes
Toxicology screen if indicated
Blood, urine, CSF cultures if indicated
LP with cell count and differential, protein, glucose, bacterial/viral/fungal cultures, cytology/flow cytometry, autoimmune/paraneoplastic panels as indicated
EEG
MRI brain with contrast depending on the clinical scenario and when the patient is clinically stable
Treatment
ABCs (airway, breathing, circulation) and consultation of ICU if the patient may require intubation and/or pressor support
Correction of metabolic derangements
Reduction of elevated ICP - raise head of the bed to 30 degrees, hyperventilation (if possible) to PCO2 35-40 mmHg, avoid hypotension, hypertonic saline 150-300 cc over 15-30 min (avoid in patients with serum Na+ >160) or mannitol 1-1.5 g/kg bolus q4-6h PRN (avoid in patients with disrupted blood brain barrier or renal dysfunction)
CIWA protocol for suspected alcohol withdrawal
Consultation of Neurosurgery or other specialties if indicated
Consultation of Poison Control depending on investigations and clinical scenario
For more information in managing specific acute level 2/ICU scenarios, please see the Level 2 Guide
(Click image to enlarge)
Source: The Calgary Guide to Understanding Disease
Prognosis for Coma
For a Decision Algorithm for Use in Outcome Prediction for Comatose Survivors of Cardiac Arrest, see Figure 2 in this article: Neurologic Prognosis after Cardiac Arrest
Indications for Ancillary Testing
Components of the brain death exam cannot be completed because of the underlying medical condition
Uncertainty about the reliability of parts of the neurologic examination
Apnea test cannot be performed
Ancillary Testing for Brain Death
CTA Head & CT Perfusion
Transcranial Dopplers
Radionuclide brain perfusion scan
End of Life Care
By Dr. Caz Zhu
Clinical Symptoms
It is important to acknowledge that prognostication is very challenging and it is impossible to predict when someone may pass away; it can be anywhere from hours to a week. Some of the common signs of a patient nearing end of life include:
Unresponsive to voice or touch
Changes in breathing, increased apnea, Cheyne-stokes breathing pattern
Mottling in the skin and cooler extremities
Anuria
Decreased/no oral intake
The purpose of the End of Life Order set is to ensure patient comfort and quality of life
End of Life Order Set
Discontinue vitals, bloodwork, telemetry , POCTs
Monitor patient q1h for comfort (e.g. pain, dyspnea)
Insert subcutaneous butterfly
Oxygen via Nasal Prongs as needed, titrate to patient comfort NOT SpO2
Diet as tolerated
Artificial saliva Q1H PRN
Discontinue all medications except the following: *
For pain: Hydromorphone 0.25 - 0.5 mg SC q1h PRN for pain (can increase up to 0.5 - 1 mg, also used for breathlessness)
For agitation/delirium: Haldol 1 mg SC q4h PRN for agitation or Methotrimeprazine 6.5 - 12.5 mg SC q4h PRN for agitation (very sedating, only use in cases where comfort is the focus)
For breathlessness: Lorazapam 0.5 mg SC q4h PRN for breathlessness or anxiety
For secretion management: Glycopyrrolate or Scopolamine 0.2 - 0.4 mg SC q4h PRN for secretions
For dry mouth: Artificial saliva spray or gel q2h for dry mouth
*Caveat - might continue medications if they provide patients with comfort (e.g. anti-epileptics to prevent further seizures, levodopa PR for Parkinson's Disease) if patient is able to tolerate the medication
Neuro-inflammatory
Autoimmune Encephalitis
By Dr. Andrea Kuczynski
Definition
Syndrome of subacute onset of neurological and/or psychiatric dysfunction affecting one or more brain systems and associated with an immune-response compromising function
Pathophysiology and Epidemiology
Peak incidence <40 years
Female predominance
60-75% of patients have a preceding infectious prodrome
Malignancy is common in up to 50% of females between 20-50 years old
Several antibodies have been identified with variable clinical presentations: anti-NMDA, anti-LGI1, anti-DPPX, anti-Caspr2, anti-GABA, anti-AMPA, anti-IgLON5, thyroid antibodies among others
Clinical Features
Altered level of consciousness/mental status
Psychosis - delusions, hallucinations
Seizures
Agitation, aggression
Catatonia
Disinhibition
Short-term memory impairment
Dysautonomia
Abnormal movements - dystonia, myoclonus, chorea, rigidity
Language dysfunction - mutism, echolalia, aphasia
Sleeping disorders - insomnia at onset, hypersomnia later
Investigations
Stat CT head to rule out acute intracranial abnormality (i.e., hemorrhage, stroke, mass lesion)
CBC
Lytes, extended lytes (Mg, Ca, PO4), creatinine
Blood glucose
Liver enzymes
TSH, free T3 and T4, and thyroid antibodies
MRI brain with contrast: may be normal or show T2/FLAIR hyperintensities or contrast uptake depending on associated antibody
LP: may see pleocytosis, normal glucose, normal to high protein
Serum and CSF autoimmune/paraneoplastic panels (see Requisition Forms section)
Autoimmune blood work: ESR, CRP, ANA, anti-dsDNA, ENA, RF, ANCA, C3/C4
HIV, VDRL [Remember to send CSF Oligoclonal bands with Serum SPEP test]
EEG if there is concern of altered mental status and/or seizures
CT chest/abdo/pelvis to assess for malignancy
Transvaginal U/S in female, testicular U/S in males to assess for malignancy
In preparation for high dose steroids: Hepatitis B and C serology, TBST, strongyloides serology
Treatment
Pulse steroids x5 days with maintenance Prednisone 1 mg/kg thereafter
IVIG 2 g/kg over 2-4 days (4 days if patient has cardiac comorbidities)
PLEX - can vary from 5-7 sessions
Second-line therapy: Rituximab, Cyclophosphamide
Management of comorbid symptoms (i.e., seizures, pain, psychosis)
Prophylaxis while on high dose steroids: calcium, vitamin D, PPI, PJP prophylaxis
Sarcoidosis
By Dr. Andrea Kuczynski
Pathophysiology and Epidemiology
Granulomatous, multisystem disease (commonly in the lungs, lymph nodes, but can also affect other organs including the brain)
Pathophysiology not well understood
Risk factors
Genetic predisposition - 5-fold higher risk with first- or second-degree relatives
High risk occupations - agriculture, healthcare, animal laboratories
Smoking
Clinical Features
Panhypopituitarism
Pulmonary involvement - dyspnea, persistent dry cough
Painless lymphadenopathy
Cardiac involvement - cardiomyopathy, chest pain, palpitations/arrhythmia, syncope
Neurological involvement - cranial nerve palsies, radiculopathy, confusion, myelopathy
Orbital involvement - dry eyes, blurry vision, visual loss, uveitis
Rashes, erythema nodosum
Arthralgias
Hepatosplenomegaly
Amenorrhea
Investigations
Elevated serum ACE level (not specific)
Elevated IgG subclasses (not specific)
Hypercalcemia
MRI brain with contrast: may have meningeal or parenchymal enhancement, involvement of cranial nerves or spinal nerve roots, spinal cord or cauda equina edema
LP: may have elevated opening pressure, may have pleocytosis, normal to low glucose, normal to high protein, elevated ACE and IgG index and increased CD4/CD8 ratio (on cytology)
CXR: hilar lymphadenopathy
Cardiac investigations: TTE, ECG, cardiac MRI
Biopsy: non-caseating granuloma
EMG/NCS if component of neuropathy
In preparation for high dose steroids: Hepatitis B and C serology, TBST, strongyloides serology
Treatment
Solumedrol 1g IV x3-5 days followed by maintenance Prednisone 1 mg/kg daily with taper
Steroid sparing agents: MTX, Azathioprine, Cyclophosphamide
Prophylaxis while on high dose steroids: calcium, vitamin D, PPI, PJP prophylaxis
Checkpoint Inhibitor Complications
By Dr. Andrea Kuczynski
Pathophysiology
3 main classes of immune checkpoint inhibitors: anti-CTLA4, anti-PD1, and anti-PDL1
Checkpoint inhibitors were initially developed for treatment of melanoma but now are used as targeted therapies against T-cell activation in many types of malignancy
Exact pathophysiology in relation to the neurological complications is unknown
Neurological involvement is rare (1-3%) but has the highest fatality alongside cardiac involvement
Symptom onset within 1-4 weeks of therapy
Clinical Features
Myasthenia gravis - fatigable proximal muscle weakness, bulbar weakness (i.e., dysphagia, diplopia, respiratory difficulties) occurring more commonly in men of older ages unlike typical bimodal distribution in idiopathic MG
Myositis - second most common complication
Polyneuropathy
Mononeuritis multiplex
Cranial nerve palsies - most commonly VI and VII
Encephalitis
Aseptic meningitis
Investigations
CK - often normal or elevated depending on presence of myopathy and/or myocarditis
Serum mitogen myositis panel
EMG/NCS - results depend on clinical presentation but may identify sensorimotor polyneuropathy, active myopathy
If there are features of myasthenia gravis: serum anti-AChR antibody and anti-MuSK antibody, single fiber EMG identifying increased jitter response
MRI brain and/or full spine depending on clinical presentation
Consider LP and assess for autoimmune/paraneoplastic antibodies depending on patient profile and clinical presentation
If there is cardiac involvement: elevated troponin, ECG, TTE, cardiac MRI
Treatment
Discontinue the offending agent and supportive care
Pulse steroids Solumedrol 1g IV daily x5 days followed by maintenance steroids of Prednisone 1 mg/kg dosing with slow taper
IVIG 2 g/kg over 2 days (4 days if cardiac comorbidities) or PLEX in patients with incomplete benefit from steroids or those with severe bulbar weakness and/or respiratory difficulties
If myasthenia gravis: trial of Mestinon 30mg p.o. TID
Patient Education
Some of the side-effects from checkpoint inhibitors are not completely reversible even with discontinuation of the inhibitor and treatment as outlined above
There is mortality benefit with early initiation of pulse steroids in those with myocardial involvement
Functional Neurological Disorders (FND)
By Dr. Caz Zhu
Reviewed by Dr. Matt Burke
Pathophysiology
Neurological symptoms due to a “functional” disruption of brain networks than a recognized “structural” disorder of the nervous system
Etiology is incompletely understood, multiple aspects of biopsychosocial model involved in the disease (e.g. genetics, childhood adverse events, acute stressors such as trauma)
Diagnostic Criteria
A diagnosis made by positive findings from physical examination and semiology
Patients do not necessarily need a psychosocial stressor or psychological trigger in making the diagnosis
Based on DMS-5 Criteria for Conversion Disorder (Functional Neurological Disorder) - patient must have altered sensory/motor symptom that is incompatible with a recognized medical/neurological condition and causes clinically significant distress or impairment in areas of functioning
Clinical Features
To learn more about FND, visit this module created by Dr. Jane Liao and Dr. Sarah Lidstone - Functional Neurological Disorders: Let's talk about it
For a full detailed list of possible clinical features: consider reading Diagnosis and Management of Functional neurological disorder by Aybek and Perez 2022
| FND sub-types | Positive symptoms |
|---|---|
| General signs | Distractible (if engaging patient on a different task, abnormal movements may stop), Variability (symptoms fluctuate during assessment or when patient is not being tested) |
| Functional tremor or movements | Entrainable (when copying rhythmic movements with hand, tremor in affected limb may stop or entrained to the same rhythm) |
| Functional gait | Falling towards support (falling towards objects that will break their fall), excessive slowness, disproportionate hesitation when walking |
| Functional weakness | Inconsistent or “give-away” weakness, Hoover’s Sign, Teapot Sign, Pinky Sign, Pronator drift without pronation |
| Functional seizures | See PNES - Long duration of waxing and waning episodes, forced eye closure, tearfulness, side-to-side head shaking, full-body tonic-clonic movements with preserved consciousness |
Investigations
Functional neurological disorder is a diagnosis made on the basis of positive signs as outlined above, however can consider investigations including bloodwork, imaging, +/- EEG/EMG if there is uncertainty about the diagnosis
Treatment
Communicating the diagnosis to the patient- critical for the patient's understanding and demonstrating positive symptoms can be helpful. Communicating the diagnosis does not mean telling the patient what diseases they don’t have or that their symptoms are “medically unexplained”
Important to validate patients’ experiences and provide education regarding the disease
Multidisciplinary approach to treatment depending on presentation e.g. some patients with motor-related FND can benefit from FND-informed physiotherapy or patients with PNES can benefit from Cognitive-behavioral therapy
Patients with co-morbid anxiety and depression (which can worsen FND) can benefit from psychotherapy and antidepressants
Patient Education
One aspect that can benefit patients is to provide them with resources to learn more about FND and speak to other people living with it - these include www.fndhope.org or www.neurosymptoms.org
Requisition Forms
Antibody/autoimmune/PNP forms
1. UHN serum autoimmune and paraneoplastic profiles - Need serum (gold or red tubes) with the miscellaneous paper requisition form and write "paraneoplastic panel and autoimmune panel"Autoimmune Liver Disease Profile (will include 9 autoantibodies): Anti AMA-M2, Anti M2-3E (BPO), Anti Sp100, Anti PML, Anti gp210, Anti LKM-1, Anti LC-1, Anti SLA/LP, Anti Ro-52Myositis Antibodies Profile (will include 16 autoantibodies): Anti Mi-2 alpha, Anti Mi-2 beta, Anti TIF gamma, Anti MDA5, Anti NXP2, Anti SAE1, Anti Ku, Anti PM-Scl 100, Anti PM-Scl75, Anti Jo1, Anti SRP, Anti PL-7, Anti PL-12, Anti EJ, Anti OJ, Anti Ro-52Paraneoplastic Disease Profile (will include 12 autoantibodies): Anti Amphiphysin, Anti CV2, Anti PNMA2 (Ma2/Ta), Anti Ri (Nova1), Anti Yo, Anti Hu, Anti Recoverin, Anti SOX1, Anti Titin, Anti Zic4, Anti GAD65, Anti Tr (DNER)2. Mitogen Autoantibody Test Requisition for Paraneoplastic/Autoimmune Panel for CSF- Link3. LHSC General Immunology and Neuroimmunology Testing Requisition for Paraneoplastic/Autoimmune Panel for CSF- Link4. SickKids Anti-NMDAR Serology requistion form - Link5. SickKids Biochemistry requisitions (e.g. Toxicology, Genomic Diagnostics) - Link6. North York General Molecular Genetics Requisition (e.g. SCA, OPMD, Fragile X) - Link7. St. Joseph's Immunology Requisition outside of Unity Health (e.g. Myositis, NMOSD) - Link8. BC Neuro Requisition (e.g. MuSK and ACHr antibodies, CIDP - for serum sample, they need gold tubes) - Link
IVIG
Ontario MOHLTC IVIG Request Form Neurology - Link
MTO reporting for driving
Ontario Medical Condition Report Form - Link
NPH Protocol
UHN NPH protocol developed by Dr. Tang-Wai and Dr. Fasano - for use at UHN but can be used as a reference guide at other sites (i.e. but should not be printed and placed in patient's chart)
About & Contact us
This resource was created by Dr. Andrea Kuczynski and Dr. Caz Zhu with support and guidance from Dr. David Chan.To contact us regarding any inquiries or feedback to improve the website (e.g. if there are any sections you would like to see), please fill out the form below.
Last updated: July 2022
Acknowledgment
We thank all the past and current residents who have generously contributed their time to this endeavor as well as faculty members who have reviewed the content. We also thank Dr. Eshita Kapoor for the conception and organization of the initial iteration of creating a resource for residents.
| Contributors |
|---|
| Dr. Elliot Cohen |
| Dr. Conrad Eng |
| Dr. Kia Gilani |
| Dr. Priti Gros |
| Dr. Andrea Kuczynski |
| Dr. Jane Liao |
| Dr. Amirah Momen |
| Dr. Calvin Santiago |
| Dr. Caz Zhu |
| Dr. Jeremy Zung |
| Faculty Reviewers |
|---|
| Dr. Matthew Burke |
| Dr. David Chan |
| Dr. Jerry Chen |
| Dr. David Fam |
| Dr. Tess Fitzpatrick |
| Dr. Will Kingston |
| Dr. Houman Khosravani |
| Dr. Alex Muccilli |
| Dr. Jonathan Micieli |
| Dr. Emily Swinkin |
| Dr. David Tang-Wai |
Disclaimer
This Terms of Use Agreement (this “Agreement”) is entered into by and between oncallneuro.ca (the “author”) and “you,” the user of this web site (the “site”). Access to, use of and/or browsing of the site is provided subject to the terms and conditions set forth herein. By accessing, using and/or browsing the site, you hereby agree to these terms and conditions.All opinions expressed here are those of their authors and not of their employer.OVERVIEW: Information provided here is for EDUCATIONAL PURPOSES ONLY. THERE IS NO DUTY OF CARE. It is not intended as and does not substitute for medical advice. If you are a patient, please see your doctor for evaluation of your individual case. Under no circumstances will the authors be liable to you for any direct or indirect damages arising in connection with use of this website. This website's intended audience are medical providers (medical students, residents, staff, RNs) for EDUCATIONAL PURPOSES ONLY. Any operational decisions or use is at the discretion of the provider and based on their expertise and personal decisions. This website and its content have no medical care responsibility and do not claim to be the ground source of truth and does not replace expert opinion and practice.The appearance of external hyperlinks to other websites does not constitute endorsement. We do not verify, endorse, or take responsibility for the accuracy, currency, completeness or quality of the content contained in these sites.Patient Data: There are photos used, taken with permission, to illustrate concepts but none of the images can be used to identify specific patients.Purpose of this web site: This web site is intended for medical professionals but can also be accessed by the general public. The information provided here is made available by the authors for educational purposes only and is not intended to provide medical advice. By accessing the web site, the visitors acknowledge that there is no physician-patient relationship between them and the authors. The web site should not be used as a substitute for competent medical advice from a licensed physician.Privacy: This web site does not collect any personal information about its visitors and readers. It does not apply cookies.Links to other web sites: This web site may contain links to third party web sites. These links do not represent a guarantee, warranty, or recommendation by the authors of this web site or an indication of any affiliation, sponsorship or endorsement of such third party web sites.(disclaimer adapted from codestroke.net)